How to diagnose and treat Lung Cancer?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
How to diagnose and treat Lung Cancer?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
How to diagnose and treat Lung Cancer?
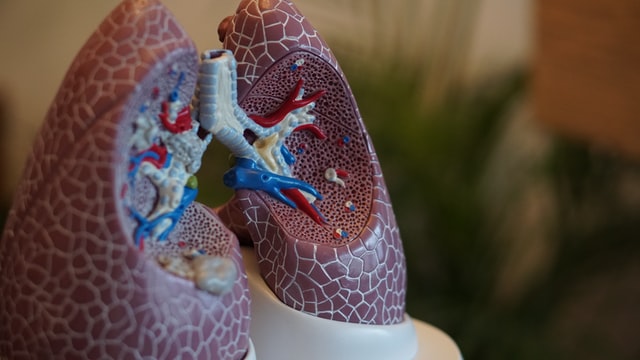
Lung cancer is a cellular disease that begins with the transformation of the epithelial cells of the lung tissue into cancerous cells, and over time, forms a primary tumor mass that grows and invades other tissues, and even spreads to the lungs and other tissues of the body of malignant tumors.
Lung cancer is known as the king of cancer, with the fastest growing morbidity and mortality , and one of the most threatening malignant tumors to the health and life of the population.
Lung cancer has no symptoms in the early stage, and it is already in the advanced stage when there are symptoms.
01 Causes of lung cancer
Lung cancer is so terrible, so how is lung cancer caused? Smoking and second-hand smoke are the main factors that cause lung cancer. Diseases such as inflammation, chronic pneumonia, and pulmonary fibrosis can also cause lung cancer.
Family genetic factors are one of the important risk factors for lung cancer. In addition, lung cancer is more prevalent in men over the age of 40 .
02 Lung cancer symptoms and screening
For many years, people have been hoping to find early lung cancer by studying the early symptoms of lung cancer, but unfortunately, there are no symptoms at all in the early stage of lung cancer.
Once symptoms appear, such as Hoarseness, shoulder pain, etc. At this time, lung cancer is not in the early stage, so it is not reliable to find early lung cancer through symptoms.
But people can find lung cancer early in other ways, and that’s cancer screening. Cancer screening is not the same as physical examination .
Many people complain: ” Physical examination is normal every year, but advanced lung cancer still comes to the door . ” This is because general physical examinations are only chest X-rays and tumor markers, and these two examinations cannot detect early lung cancer .
Dose spiral CT ( Low-dose computed tomography , LDCT ), which is currently known as the best screening method for early detection of lung cancer.
03 Screening population
Lung cancer screening should be carried out in high-risk groups of lung cancer . People at high risk of lung cancer are between ( 50-74 ) years old and meet at least one of the following conditions :
3.1. The number of smoking pack years [ the number of smoking packs per day ( 20 packs per pack) × the number of smoking years ] is not less than 30 (pack years), including not less than 30 (pack years) of smoking, but less than 15 years after quitting smoking;
3.2. Living or working in the same room as passive smoking for more than 20 years ;
3.3. Have a history of chronic obstructive pulmonary disease ( COPD ) or diffuse pulmonary fibrosis ;
3.4. Have a history of occupational exposure for not less than one year, including exposure to asbestos, radon, beryllium, chromium, cadmium, silicon, soot and soot;
3.5. Have first-degree relatives (parents, children and siblings) diagnosed with lung cancer.
04 Screening results of low-dose spiral CT (LDCT)
Low-dose spiral CT is a commonly used type of CT examination in clinical practice. The scan is based on ordinary CT , and it is a way to reduce the scanning parameters .
For example, it reduces the tube current and tube current sample, It is precisely because of the optimized parameters that the radiation dose to the human body is relatively low, and it is usually used for crowd screening or inspection of people who are sensitive to radiation.
Low-dose chest CT is the most effective way to detect early lung cancer, its sensitivity is 4-10 times that of conventional chest X-ray, and it can detect early peripheral lung cancer .
According to data from the International Early Lung Cancer Action Plan, low-dose chest CT annual screening can detect 85% of stage I peripheral lung cancers, and the expected 10- year survival rate after surgery is 92% , which can reduce the overall lung cancer mortality rate by about 20% .
The management and follow-up of baseline screening results should comply with the following regulations:
4.1. If no non-calcified nodules in the lungs are detected (negative) , then enter the screening in the next year;
4.2. If the average diameter of the detected non-solid nodules is < 8.0 mm , or the average diameter of the solid component of the solid nodules / part-solid nodules is < 6.0 mm , then enter the screening in the next year;
4.3. Detected 6.0 mm ≤ solid nodules or the average diameter of the solid component of part-solid nodules < 15.0 mm , or 8.0 mm ≤ the average diameter of non-solid nodules < 15.0 mm , should be reexamined after 3 months; For solid nodules or part-solid nodules, if the radiologist believes that they have clear malignant features, multidisciplinary consultation should be carried out, and clinical intervention should be decided according to the consultation opinions.
4.4.The average diameter of detected solid nodules, solid components of part-solid nodules, or non-solid nodules is not less than 15.0 mm , and the following two options should be selected:
( a ) Re-examination one month after anti-inflammatory treatment or one month after anti-inflammatory treatment is not required . During the re-examination, treatment and follow-up will be carried out according to the following conditions: (1) If the nodule is completely absorbed, it will be screened in the next year; ( 2 ) The section is partially absorbed, and it is advisable to check again after 3 months. During the re-examination, if the nodules are partially absorbed and do not increase again, they will enter the next year’s screening; if the nodules are partially absorbed and then increase, it is advisable to conduct multidisciplinary consultation, and decide whether to perform clinical intervention according to the consultation opinions; (3 ) Nodules If it has not shrunk, it is advisable to conduct multidisciplinary consultation, and decide whether to perform clinical intervention or reexamination after ( 3 to 6 ) months according to the consultation opinion;
( b ) Biopsy or PET-CT examination for solid and part-solid nodules , and treatment and follow-up according to the following conditions:
- If it is positive, it is advisable to conduct multidisciplinary consultation, and decide whether to perform clinical intervention according to the consultation opinion;
- If it is negative or indeterminate, it should be re-examined after 3 months. If the nodules remain unchanged or increase during reexamination, multidisciplinary consultation should be carried out, and clinical intervention should be decided according to the consultation opinions; if the nodules shrink, screening will be carried out in the next year.
4.5.Suspected airway lesions, such as lumen occlusion, stenosis, irregular and thickened tube walls; abnormal soft tissue shadows of the hilum closely related to the bronchi; suspicious obstructive inflammation, atelectasis and bronchial mucus plugs, etc. Perform sputum cytology or fiberoptic bronchoscopy, and conduct treatment and follow-up according to the following conditions:
( a ) If it is positive, multidisciplinary consultation should be carried out, and clinical intervention should be decided according to the consultation opinion;
( b ) Negative, enter the next annual screening.
4.6. The principle of treatment of multiple pulmonary nodules is based on the principle of treatment of the most serious lesions.
05 Lung Cancer Diagnosis
There are no symptoms at all in the early stage of lung cancer. Once symptoms appear, such as irritating dry cough, bloody sputum, difficulty breathing, hoarseness and shoulder pain, etc., you should go to the hospital for examination in time. Hospital diagnoses generally include:
5.1. Laboratory examinations such as blood routine, liver and kidney function and other necessary biochemical and immune tests and coagulation function tests.
5.2. Serological tumor marker detection : Currently, the commonly used primary lung cancer markers recommended by the American Committee of Clinical Biochemistry and the European Tumor Marker Expert Group include carcinoembryonic antigen ( CEA ), neuron-specific enolase ( NSE ), cell Keratin 19 fragment ( CYFRA21-1 ) and gastrin-releasing peptide precursor ( ProGRP ), and squamous cell carcinoma antigen ( SCCAg ), among others. The combined use of the above tumor markers can improve their sensitivity and specificity in clinical application.
During clinical diagnosis, tumor markers related to lung cancer can be detected as needed, auxiliary diagnosis and differential diagnosis can be made, and the possible pathological types of lung cancer can be understood.
a. Small cell lung cancer ( SCLC ): NSE and ProGRP are ideal indicators for auxiliary diagnosis of SCLC .
b. Non-small cell lung cancer ( NSCLC ): In patients’ serum, elevated levels of CEA , SCC , and CYFRA21-1 are helpful for the diagnosis of NSCLC . It is generally believed that SCC and CYFRA21-1 have higher specificity for squamous cell carcinoma of the lung.
If NSE , CYFRA21-1 , ProGRP , CEA and SCCAg and other indicators are combined to detect , the accuracy of distinguishing SCLC and NSCLC can be improved.
5.3. Imaging examination
Imaging examination methods for lung cancer mainly include: chest X -ray, CT , MRI , ultrasound, radionuclide imaging, PET-CT and other methods. It is mainly used for lung cancer diagnosis and differential diagnosis, staging and re-staging, evaluation of surgical resectability, efficacy monitoring and prognosis evaluation, etc. Imaging examination is the best method for non-invasive detection and evaluation of tumors. Imaging information enables clinicians to be more confident in judging tumor prognosis and making treatment decisions. In the diagnosis and treatment of lung cancer, one or more imaging examination methods should be selected reasonably and effectively according to different examination purposes.
06 Lung Cancer Staging
Lung cancer staging is a doctor’s assessment of how far the cancer has progressed and spread. Doctors then plan further tests and treatments depending on how advanced the cancer is.
Therefore, staging is very important for the formulation of treatment plans. Everyone’s condition is different, and no single stage is suitable for everyone.
In terms of large types, lung cancer can be divided into small cell lung cancer and non-small cell lung cancer. On the whole, the treatment effect of small cell lung cancer is far worse than that of non-small cell lung cancer.
The severity of non-small cell lung cancer depends on its stage. Early, middle, and late stages are just general terms, and there are more scientific description methods in medicine.
The TNM staging system is most commonly used to describe the extent to which NSCLC has grown and spread .
Tumor ( T ) – represents the primary tumor and describes the size of the tumor and how far the cancer has spread into the lung tissue.
Tumors can be graded from T1a (describes tumors smaller than 1 cm ) to T4 (describes tumors larger than 7 cm ) .
Lymph (N) – stands for nodal spread and describes whether the tumor has spread to nearby lymph nodes. Lymph can be graded from N0 (indicating no spread) to N3 (indicating cancer has spread to other parts of the body, such as the chest or the other side of the collarbone).
Metastatic (M) – Describes whether the cancer has spread to other areas of the body other than the lungs . The metastatic grade ranges from M0 (meaning it has not spread) to M1c (meaning the cancer has spread to other organs in the body and created more tumors).
Due to the characteristics of rapid progression and early metastasis of small cell lung cancer, a two-stage system is more commonly used clinically, that is, small cell lung cancer is divided into limited stage and extensive stage .
07 Lung Cancer Treatment
Early detection of lung cancer is of great significance to the treatment of lung cancer.
The vast majority of early lung cancer can be effectively controlled through treatment.
If early lung cancer is found, you should choose a regular hospital for standardized clinical treatment.
For early non-small cell lung cancer Patients should strive for surgical resection to obtain the best curative effect .
At this time, the focus of treatment is fast and early. The earlier the diagnosis, the faster the treatment, the better the effect and the greater the possibility of recovery.
For locally advanced disease, it should be a comprehensive treatment that combines multiple treatment options, such as surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy.
If it is properly controlled and metastasis is avoided, the survival rate will be greatly improved.
For patients with distant metastases, active treatment should also be taken, mainly systemic treatments such as chemotherapy, targeted therapy, and immunotherapy. At this time, confidence is far lower than The treatment itself is more important .
For lung cancer patients, early low-dose spiral CT examination is particularly important . Early screening, early treatment, and early recovery.
Generally speaking, for the prevention of lung cancer, high-risk groups should actively do cancer screening in addition to improving their own environment.
In addition, smoking cessation is as important as screening, numbers will not lie, after all, life insurance is only once,
Targeted therapy and immunotherapy drugs are the two mainstream drugs for the treatment of lung cancer, among which targeted therapy drugs are divided into small molecule and macromolecule drugs.
Small-molecule targeted therapy drugs are mainly used for the treatment of EGFR , ALK , MET mutations and other NSCLC .
Large-molecule targeted therapy drugs mainly refer to VEGF/VEGFR monoclonal antibodies .
Immunotherapy drugs are a better choice for patients without obvious driver genes. Mainly refers to PD-1/PD-L1 .
08 Targeted therapy drugs
Targeted therapy is a cancer treatment that uses drugs designed to ” target ” cancer cells without harming normal cells.
The side effects of targeted drugs are far less than that of chemotherapy, and the curative effect is far better than that of chemotherapy.
While improving the survival time of patients, the quality of life can also be maintained.
In layman’s terms, chemotherapy is low-efficiency and high-toxicity, while targeted drugs are high-efficiency and low-toxicity.
According to statistics from the National Cancer Center, there were 780,000 new lung cancer patients in China in 2015 , with an annual growth rate of 2%-3% , of which 85% were non-small cell lung cancer (including lung adenocarcinoma, squamous cell carcinoma, and large cell undifferentiated carcinoma). etc.), among which the EGFR gene mutation ratio was 28.20% , KRAS mutation ratio was 6.00% , ALK was 5.60% , and ROS1 was 1.90% .
For non-small cell lung cancer with activating EGFR mutations, great progress has been made in targeted therapy, including EGFR- targeted small molecule drugs and monoclonal antibodies.
At present , 4 generations of EGFR -targeted small molecule drugs have been developed , 1-3 generations of targeted drugs have been widely , and the fourth generation of targeted drugs is already undergoing clinical trials .
First-generation drugs include gefitinib, erlotinib, and icotinib ; second-generation drugs include afatinib and dacomitinib ; third-generation drugs include osimertinib, amitinib, and Metinib .
The use of these drugs will inevitably produce resistance mutations. The main resistance mutation of the third-generation drugs is also C797S , which needs to be overcome by the fourth-generation EGFR -targeted drugs.
The first three generations of inhibitors all target the catalytic site, and the fourth-generation is the targeted allosteric site .
There are many fourth-generation drugs under development, but most of them are in the early research stage. At present, only two drugs have published preliminary human trial data, namely BLU-945 and BBT-176 .
However, EGFR is a mutation-prone gene, and resistance to these small molecule drugs targeting EGFR will appear sooner or later, so new technologies such as protein degradation targeting chimeras (PROTACs) and lysosome targeting chimeras are needed (LYTACs) and antibody-drug conjugates (ADCs) , etc.
①Protein degradation targeting chimera (PROTACs) : It is a very popular technology in recent years .
It includes three parts, one part binds the target protein, the other part binds E3 ligase and the connecting chain connecting the two parts.
Many EGFR PROTACs have been reported, including CRBN ligand-based PROTACs , VHL ligand-based PROTACs , IAPs -based PROTACs and EGFR / PARP dual-targeted PROTAC degraders.
On January 10 , 2023 , the clinical trial application of HSK40118 , an oral EGFR-PROTAC small-molecule anti -tumor drug independently developed by Haisco, was accepted by the State Drug Administration , becoming the first domestic pharmaceutical company to apply for EGFR PROTAC clinical trials.
C4 Therapeutics, a foreign company , is relatively advanced in the layout of EGFR PROTAC , and its degradation agent CFT8919 targeting EGFR L858R mutation has been applied for clinical application.
However, EGFR PROTAC drugs are still in the early clinical stage, and it will take time to prove whether they can successfully solve the problem of EGFR drug resistance.
Recently, Malek et al. reported PROTACs of EGFR different from the conventional concept in cell chemical biology .
It was previously believed that PROTACs need to recruit E3 ligase to the vicinity of the target protein to form a stable ternary complex, but Malek et al. found that E3 ligase and EGFR do not need to form a stable protein – protein interaction , and PROTAC can also be degraded EGFR 1 .
They observed a strong destabilization of mutant EGFR in the ternary complex relative to the ligand-bound state ( 0 < PF < 1 ).
This implies that the EGFR : GNE-579 interface must rearrange to form a ternary complex with VBC , which results in a free energy gain relative to EGFR .
This also implies that EGFR and VBC do not directly interact but are loosely linked through GNE579 , supporting the idea that stabilizing PPI may not be a requirement for a productive ternary complex.
②Lysosome targeting chimeras ( LYTACs ) :In 2020 , Bertozzi et al developed a novel approach called lysosome-targeting chimeras ( LYTACs ) to facilitate the degradation of extracellular proteins, including secreted proteins, cell surface receptors and membrane proteins, via lysosomes way.
The LYTAC system consists of two main parts, one part is the specific antibody corresponding to the substrate protein to be degraded, which can specifically bind the substrate protein to be degraded; the other part is capable of interacting with lysosome targeting receptors ( LTRs ) The combined NCA glycan peptides ( n=20~90 ) containing M6P branches ensure that the substrate protein at the other end can enter the lysosome along with the LTR and then complete the degradation.
Bertozzi et al. chose the FDA -approved EGFR antibody drug cetuximab to make LYTAC , which resulted in 70% degradation of EGFR in HeLa cells .
In second-generation LYTACs , the trifunctional N- acetylgalactosamine ( tri-GalNAc ) motif that binds to the novel receptor , asialoglycoprotein receptor ( ASGPR ), was incorporated via a DBCO- azide-based click reaction Fusion with cetuximab.
This ligand-based cetuximab not only exhibited comparable EGFR degradation to the first generation, but also achieved cell type selectivity.
The design of LYTACs enhances the inhibition of membrane / extracellular proteins and brings about a revolution in antibody-based therapeutics2 .
③ Antibody -drug conjugates ( ADC ) : A class of emerging drugs that combine two components of antibody and small molecule cytotoxin , including humanized / humanized monoclonal antibody ( mAb ), cytotoxic load ( Cytotoxic payload or warhead ) and linker ( Linker ) are composed of three parts.
The EGFR target is a relatively hot target in ADC drug research. There are more than 20 EGFR -ADC projects in the world, and the competition is relatively fierce.
The monoclonal antibody “40H3” binds to EGFR vIII and full-length EGFR when overexpressed on cancer cells .
To generate candidate cytotoxic antibody – drug conjugates ( ADCs ), Antignani et al. by adding small molecular weight payloads including two tubulin modifiers, two topoisomerase inhibitors, and pyrrolylbenzodiazepines Class ( PBD ) dimers modify 40H3 .
The conjugate retained comparable antigen binding activity to the unmodified 40H3 antibody.
The cytotoxicity of five different ADCs was evaluated on a variety of EGFR – expressing cells, and the 40H3 conjugate with PBD dimer ( 40H3-Tesirine ) was found to be the most active killer.
The killing of EGFR- positive cells by 40H3-Tesirine correlates with the number of surface binding sites of 40H33 .
In addition to targeting EGFR mutant proteins, it is also a targeted therapeutic drug targeting ALK , ROS1 , MET , K RAS and other mutant proteins .
Genetic testing must be done first ( genetic testing refers to the detection of gene mutations on the patient’s tumor tissue, pleural effusion or blood samples, to detect whether there are abnormal mutated genes , some abnormal mutated genes lead to the development of tumors, and promote Intrinsic factors of its growth) , and then use targeted drugs, only with the genetic test report, can targeted drugs be used , unless there is no chance to obtain pathological specimens (patients with poor physical fitness take targeted drugs blindly.
If there is no opportunity to obtain pathological specimens , you can also consider using liquid biopsy for genetic testing, liquid biopsy mainly uses blood samples for genetic testing) on the basis of gene mutations, select targeted drugs, the effective rate of targeted therapy for lung cancer is generally 80-90 % above.
09 Immunotherapy drugs
Immunotherapy is gradually becoming a ” specific ” drug for the treatment of advanced non-small cell lung cancer. Immunotherapy represented by immune checkpoint inhibitors (such as PD-1 monoclonal antibody or PD-L1 monoclonal antibody, etc.) has been proven to improve the survival rate of lung cancer patients .
At present, multiple PD-1 monoclonal antibodies and / or PD-L1 monoclonal antibodies have been approved for marketing and applied to the treatment of advanced and locally advanced NSCLC and SCLC , and more clinical indications are still being explored.
Immunotherapy also has its own limitations : when it was first used, the efficiency of a single drug was not particularly high, and combination therapy can improve the efficiency and overcome drug resistance; some lung cancer patients cannot benefit from immunotherapy, and it is only effective for some patients efficient.
Which patients can benefit in the long-term, which patients cannot benefit in the long-term, and how to control the tumor for those who cannot benefit in the long-term, need to be solved urgently, which is the key to tumor immunotherapy.
At present , there are many approved PD-1/L1 drugs at home and abroad.
In addition to the newly approved combination therapy of slulimumab and tremelimumab, 12 PD-1/L1 drugs have been approved globally. Approved for non-small cell lung cancer.
10 anti-vascular drugs
Currently approved anti-angiogenic drugs for non-small cell lung cancer include three categories: macromolecular monoclonal antibodies (bevacizumab, ramucirumab) targeting VEGFA or its receptor VEGFR ; Small-molecule TKI drugs (anlotinib) that mainly inhibit downstream signals of the VEGF pathway; and recombinant human endostatin with pan-targets.
11 Small Cell Lung Cancer
Although small cell lung cancer is a type of lung cancer, it has completely different characteristics from common lung cancer. Strictly speaking, small cell lung cancer is a systemic disease .
In the traditional treatment mode, the treatment of small cell lung cancer mainly relies on chemotherapy and radiotherapy .
With the development of immunotherapy, the treatment mode of small cell lung cancer has undergone some changes.
The two immunotherapy drugs currently approved for small cell lung cancer are PD-L1 inhibitors, namely atezolizumab (which has entered the medical insurance) and durvalumab .
In March 2019 , the FDA approved atezolizumab (Taishengqi, T medicine) combined with chemotherapy drugs carboplatin and etoposide for the first-line treatment of extensive-stage small cell lung cancer. T drug is the first immunotherapy drug approved for the first-line treatment of small cell lung cancer.
In March 2020 , durvalumab (Infinity, I drug) was approved by the FDA for first-line use in extensive-stage small cell lung cancer.
In August 2018 , the FDA approved the PD-1 inhibitor nivolumab as a third-line treatment for small cell lung cancer. This is the first new drug in the field of small cell lung cancer in 20 years.
However, in December 2020 , the indication of drug O for small cell lung cancer was withdrawn due to the successive failures of the confirmatory phase III clinical trials CheckMate 331 and CheckMate 451 .
In June 2019 , the FDA approved K drug for the third-line and above treatment of small cell lung cancer in patients with metastatic small cell lung cancer.
However, the results of the KEYNOTE-604 phase III clinical study showed that pembrolizumab combined with chemotherapy in the first-line treatment of small cell lung cancer can reduce the risk of disease progression ( 4.5 months vs 4.3 months), but there is no significant difference in OS .
For this reason, on March 1 , 2021 , Merck voluntarily withdrew the third – line indication of pembrolizumab for extensive-stage small cell lung cancer .
Small cell lung cancer rarely has sensitive gene mutations, so it is impossible to have as many targeted drugs as adenocarcinoma.
At present, the targeted drug recommended by the guidelines is only the multi-targeted anti-angiogenic drug anlotinib , which is recommended as a third-line or above drug.
12 Prevention of lung cancer
In a sense, lung cancer is the most preventable cancer . Because the occurrence of lung cancer is closely related to unhealthy lifestyle, and it is the most definite cause of various cancers.
Therefore, we can say that lung cancer is ” preventable and curable ” . Changing unhealthy lifestyles and habits, avoiding and reducing contact with various risk factors are the key to preventing lung cancer.
12.1. Stay away from tobacco : Smoking is the number one cause of lung cancer. Stay away from tobacco, not only refers to not smoking, but also stay away from second-hand smoke and third-hand smoke, even in public places, you should try to avoid being affected;
12.2. Reduce the inhalation of lung cancer-causing substances (inorganic arsenic, asbestos, chromium, nickel in industrial and mining industries, coal coke, tar and coal combustion products such as 3 , 4- benzopyrene, etc.) . Workers in a dust-polluted environment should wear masks or other protective masks to reduce the inhalation of harmful substances;
12.3. Maintain a good indoor environment : Use environmentally friendly materials for decoration as much as possible. Radon is a known substance that causes lung cancer, and the home should be well ventilated;
12.4. Maintain a healthy attitude and check your body regularly ;
12.5. Reasonably strengthen nutrition ;
12.6. Healthy cooking, less cooking fumes, clean and ventilated kitchen as much as possible, and use high-efficiency range hoods ;
12.7. High-risk groups need to strengthen their awareness of physical examination and regularly participate in lung cancer screening .
References
1. Scott C. Rosenberg, Frances Shanahan, Sayumi Yamazoe, Marc Kschonsak, Yi J. Zeng, James Lee, Emile Plise, Ivana Yen, Christopher M. Rose, John G. Quinn, Lewis J. Gazzard, Benjamin T. Walters, Donald S. Kirkpatrick, Steven T. Staben, Scott A. Foster, and Shiva Malek1, Ternary complex dissociation kinetics contribute to mutant-selective EGFR degradation, Cell Chemical Biology 30, 175–187, February 16, 2023.
2. G. Ahn, SM Banik, CL Miller, NM Riley, JR Cochran, CR Bertozzi, LYTACs that engage the asialoglycoprotein receptor for targeted protein degradation Nat. Chem. Biol., 17 (2021), pp. 937-946.
3. Eric Chun Hei Ho, Rong Qiu, Ellis Miller, Maria Teresa Bilotta, David FitzGerald, Antonella Antignani, Antibody drug conjugates, targeting cancer-expressed EGFR, exhibit potent and specific antitumor activity, Biomedicine & Pharmacotherapy 157 (11404)
How to diagnose and treat Lung Cancer?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



