What are Major Classes of T Cell Antigens in cancer immunotherapy?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
What are Major Classes of T Cell Antigens in cancer immunotherapy?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What are Major Classes of T Cell Antigens in cancer immunotherapy?
In recent years, cancer immunotherapy has achieved great breakthroughs, bringing considerable clinical benefits.
However, although various immunotherapy modalities exist, these have largely focused on tumor-targeting cytotoxic T cells ( CTL ).
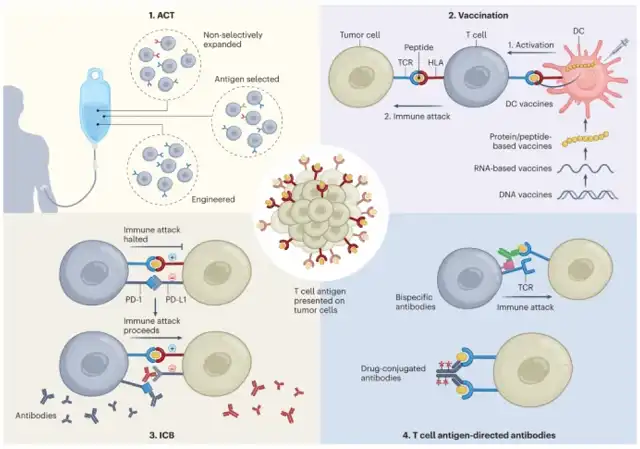
T cells are activated through specific T cell receptor ( TCR )-antigen interactions.
V(D)J recombination can generate a huge diversity ( theoretically up to 1015 ) T cell clones in the thymus , each with its unique TCR.
Further selection through positive and negative selection processes eventually yields approximately 10 6 – 10 10 circulating T cell clones.
T cell antigens are present on two major histocompatibility complex ( MHC ) molecules, called human leukocyte antigens ( HLAs ).
MHC class I molecules are expressed by all nucleated cells, while MHC class II molecules are expressed by antigen-presenting cells ( APCs ), epithelial cells, and some tumor cells.
Peptides present on MHC-I are mainly derived from intracellular proteasomal degradation products and recognized by CD8+ CTLs, whereas peptides present on MHC-II are derived from degradation by the endosomal/lysosomal system and recognized by CD4+ T cells foreign or membrane proteins.
In addition, there is a process of cross-presentation of T cell antigens, that is, tumor-exogenous peptides are mainly presented on MHC-I by XCR1+CD103+1 dendritic cells ( DC1s ), and then migrate to tumor-draining lymph nodes and trigger T cells to fight against tumor antigens . Cross-presentation is critical for CD8+ T cell priming and maturation of tumor-recognizing CTLs.
It is generally believed that tumor immune rejection is mediated by T cells, and anti-tumor T cell responses are antigen-specific. Advances in immunotherapy and available methods for T-cell antigen identification have led to a surge of interest in identifying and characterizing T-cell antigens presented by tumors , shifting to previously Sources of cancer antigens that are not widely accepted, such as non-standard and bacterial proteins.
Autoantigen
Tumor-associated autoantigens are non-mutated proteins that exhibit differential expression patterns in tumors. For example, MART-1, gplOO, and tyrosinase are tissue-specific antigens expressed in melanoma.
Tebentafusp, a bispecific fusion protein consisting of a soluble gp100-specific TCR fused to an anti-CD3 effector molecule, has clinical benefit in patients with uveal melanoma and has been approved by the U.S. Food and Drug Administration (FDA ) .
It demonstrates the potential of self-antigen-targeted therapy, however, given that tumors often have similar gene expression patterns to their tissue of origin, the use of tissue-specific antigens in therapy is limited by collateral damage to surrounding healthy tissue.
Cancer germline antigens represent another class of autoantigens, derived from proteins expressed only in germline tissues ( fetal testes and ovaries ) and trophoblast cells. In most healthy tissues, germline genes are epigenetically silenced by promoter methylation. However, in many human cancers, promoter demethylation reactivates their expression.
Analysis of 153 cancer germline genes showed that their abnormal expression was highest in skin cancer, lung cancer, liver cancer and brain cancer.
Compared with other types of autoantigens, their unique expression patterns are less affected by central immune tolerance, combined with their high prevalence in patients, making them very interesting targets for immunotherapy.
However, their expression in tumors is heterogeneous due to varying DNA methylation status.
Neoantigens derived from genomic alterations
Mutation-derived neoantigens are characterized by cancer-associated sequence aberrations encoded by somatic point mutations, frameshifts, or chromosomal aberrations.
Non-synonymous mutations leading to abnormal proteins can generate bona fide TSAs , and their degradation may lead to HLA binding of new peptides.
Single amino acid changes may alter the immunogenicity of HLA- binding peptides or, if they occur at anchor positions, convert non-binding sequences to HLA- binding sequences.
In addition, mutated amino acids can create new proteasomal cleavage sites, allowing reprocessing of peptides and loading by HLA .
The advent of next-generation sequencing has enabled systematic and comprehensive surveys of mutations in individual tumors.
In turn, these data can guide antigen discovery through T cell-based assays or HLA peptidomics.
Many neoantigens derived from recurrent mutations have been identified, such as CDK4.R24C, KRAS.G12V/C/D, EGFR, and PIK3CA.H1047L.
Less common types of mutations, such as insertions/deletions, translocations, and inversions, may also generate neoantigens.
In an analysis of three independent melanoma cohorts, frameshift/insertion mutations were found to be significantly associated with anti-PD-1 or anti-CTLA-4 responses.
Furthermore, the analysis revealed that frameshift mutations form a potentially more potent neoantigenic landscape than an equivalent number of nonsynonymous single-nucleotide variants ( nsSNVs ).
Finally, fusion genes, such as the BCR–ABL fusion in leukemia ( Philadelphia chromosome ) and the EML4–ALK fusion in non-small cell lung cancer ( NSCLC ), have been shown to generate neoantigens recognizable by T cells.
Tumor antigens from noncanonical transcription and posttranscriptional aberrations
Accumulating evidence indicates that translation of non-coding genes occurs frequently in tumors and that antitumor immune responses can target tumor antigens from non-coding regions.
Combining HLA peptidomics, RNA-sequencing, and ribosome-sequencing data uncovered hundreds of shared and tumor-specific genes derived from lncRNAs, pseudogenes, transposable elements, untranslated regions (UTRs) of coding genes, and alternative open reading frames Non-canonical HLA-presenting peptides.
Examples of antigen-specific T cell responses to intronic sequences are the N-acetylglucosaminyltransferase V gene intron, the incompletely spliced intronic region of gp100, and the 5′UTR region of the c-akt oncogene.
Examples of immunogenic MHC-presented peptides derived from alternative reading frames include NY-ESO, HER2, telomerase reverse transcriptase, prostatic acid phosphatase, and nuORFs with non-AUG translation initiation sites.
Translational reprogramming and impaired translational fidelity in cancer cells can generate non-canonical translated peptides and potentially new immunogenic antigens.
This neoantigen originates from several translational disturbances, such as ribosomal frameshifting during amino acid deprivation, oxidative stress, or codon misreading by deregulated transfer RNAs.
Finally, post-translational modifications ( PTMs ) can be deregulated in cancer cells to confer a growth advantage, which also provides potential targets for cancer immunotherapy.
However, whether these PTM-derived antigens elicit meaningful T cell responses remains to be determined.
Pathogen-derived tumor-associated antigen
Pathogen-derived TAAs are the remnants of bacterial or viral infection. If the acute infection is not cleared properly, the virus may remain inside the host cell and mediate malignant transformation.
Pathogens that can directly cause cancer include Helicobacter pylori, human papillomavirus ( HPV ), and hepatitis B and C viruses ( HBV and HCV ), among others. Induction of specific T cell responses against pathogen-derived antigens emerges as a promising strategy to elicit immune responses against cancer cells.
For example, bacterial peptides from within different tumors were found to be present on HLA molecules in patients and trigger antigen-specific immune responses in melanoma.
Antigens derived from other types of microbiomes, such as viromes , may have an intrinsic ability to elicit T cell responses, or cross-react with other TAAs in the form of molecular mimics. A classic example is the prophage-encoded antigen TMP1, which activates T cells that respond to PSMB4.
Enterococcus strain 13144 carries phages and is abundant in lung and kidney cancers, and the presence of prophages in human patients has been associated with response to immunotherapy.
Another possible source of pathogen-derived antigens is human endogenous retroviruses, and about 5% of human cancers, especially cervical and oropharyngeal malignancies, involve high-risk HPV strains. ERVE-4, whose expression is associated with immunotherapy response in clear cell renal cell carcinoma.
Finally, the recent discovery of fungi in tumors of diverse composition may suggest that fungal-derived antigens may be another tumor antigen. Whether they can trigger T cell reactivity remains to be studied.
references:
1. The landscape of T cell antigens for cancer immunotherapy. Nat Cancer. 2023 Jul 6.
What are Major Classes of T Cell Antigens in cancer immunotherapy?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



