What have we learned from ADC (Antibody-drug conjugate) development?
- Brief Intermittent Exercise Reduces Heart Disease and Death Risk
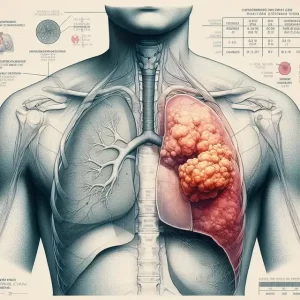
- Personalized Lung Tumor Chips Assess PD-1 Therapy Response
- Study Shows Prior Infection Offers Strong Immunity to Original COVID-19 Strain
- Chinese Food Products Dominate Korean Tables Amid Safety Concerns
- Early Detection of Hypopharyngeal Cancer Possible with Saliva Diagnosis
- EB Virus Could Be Infected by Kiss: A Hidden Threat Linked to Cancer
What have we learned from ADC (Antibody-drug conjugate) development?
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What have we learned from ADC (Antibody-drug conjugate) development?
Antibody-drug conjugate ( ADC ) is composed of a monoclonal antibody targeting a specific antigen and a small-molecule cytotoxic drug through a linker, which has both the powerful killing effect of traditional small-molecule chemotherapy and the tumor targeting of antibody drugs.
After nearly 30 years of development since first entering clinical trials in the mid-1990s, ADCs have become a very successful oncology platform.
As of January 2023, the U.S. Food and Drug Administration ( FDA ) has approved 15 ADC drugs, more with novel targets approved in the past few years than antibody-based novel immunotherapy targets ADCs (TF, Nectin-4, CD19, Trop-2, BCMA, CD79b, etc.).
However, ADCs currently under development still face many challenges that have emerged with alarming frequency and have largely hindered clinical progress.
Based on this, this article summarizes the successes and failures obtained in ADC clinical trials.
In order to obtain a faster and safer way for the development of more ADC drugs in the future.
Considerations in Experimental Protocol Design
Choose the right subject
In Phase 1 studies, too much is designed to select near-perfect patients who are more likely to respond, ignoring the stated goal of Phase 1 to establish a safe dose for the oncology patient population. In fact, eligibility is so restrictive that the search for study patients is slow, and the results are often not applicable to the typical patient in need. Therefore, the eligibility selection criteria should reflect the “real” patients who need clinical trials.
Some patients with organ dysfunction should be allowed
The population entering the Phase 1 study typically has physical and biochemical symptoms of refractory and advanced disease. In addition, these cancer patients are often elderly and also suffer from diseases related to certain organ dysfunction such as hypertension, diabetes and chronic obstructive pulmonary disease.
If preclinical toxicology does not indicate hepatic or renal toxicity, the study protocol should allow for some degree of dysfunction of these organs. Serum creatinine levels up to and including 1.5 times the upper limit of normal ( ULN ) and hepatic transaminases up to 3 times the ULN in the absence of liver metastases are generally recommended. For patients with liver metastases, it is recommended to use 5 times the ULN for patients with liver metastases.
Do not exclude patients with elevated alkaline phosphatase , as alkaline phosphatase may be of bone or hepatic origin, with little real impact on tolerability if bilirubin and hepatic transaminases are acceptable. Patients with prostate, lung, and breast cancers may have been unnecessarily excluded due to their high rate of bone metastases and elevated alkaline phosphatase.
Do not exclude patients on the basis of serum albumin levels , as there is no evidence that an albumin level of 2.8 is more meaningful than 3.0 in clinical studies. Since albumin levels are inversely correlated with tumor burden, patients with a smaller tumor burden may be inadvertently selected. This limitation will lead to significant bias.
Avoid unfounded special standards
One study arbitrarily excluded patients with oxygen saturation below 93% on room air. The standard does not specify whether it is at rest or active. Although the rationale is to reduce the risk of developing severe lung toxicity, there are no data from preclinical toxicology studies of lung injury for this molecule or payload. Furthermore, there is no known evidence that pre-study oxygen saturation predicts lung toxicity of ADCs. However, this exclusion criterion certainly excludes many patients with lung cancer, patients with underlying COPD, and patients with lung metastases.
The use of anticoagulants and some degree of abnormal coagulation parameters should be allowed. Thrombotic events are common in many cancer indications and can be well controlled and prevented with factor Xa inhibitors. Unless thrombocytopenia is predicted as a toxicity associated with the selected ADC, limiting patients to no anticoagulants or requiring normal coagulation parameters would exclude some excellent candidates.
In addition, decreased absolute lymphocyte count ( ALC ) is a common finding in patients with advanced cancer. The clinical impact of this laboratory finding in most patients is minimal, and there is generally no benefit in restricting patients with low ALC from entering the study. The strongest evidence against restricting ALC is the first clinical trial of pembrolizumab. Even in this highly successful immunotherapy, ALC criteria are not used and therefore should not be included in ADC development programs.
Do not rule out previous ADC healers
Such screening criteria, which have been observed in some newer regimens, are neither in line with contemporary drug development standards nor are they increasingly realistic as many ADCs have been approved or are in clinical development in recent years.
A common rationale for choosing to exclude prior ADC therapy is that by excluding patients with prior exposure to ADCs, the risk of acquired resistance to newer ADCs can be reduced. However, the reasons why patients do not respond to ADCs are multifactorial, including patients receiving dose levels that are too low, tumors that express too low levels of the target antigen, linker instability, or tumors that are inherently resistant to the payload. Furthermore, excluding patients who received the same payload may not be entirely valid, as sporadic patient responses have been observed in ADCs with similar ADC payloads in the past.
New treatments must address unmet patient needs, and the most valuable and fastest pathways to approval are based on benefit for patients who have failed prior treatments. Accelerated approval of trastuzumab deruxtecan ( Enhertu® ) for HER2-positive metastatic breast cancer is a case in point. The study specifically included patients with HER2-positive breast cancer who had failed treatment with trastuzumab-emtansine ( Kadcyla® ). Significant response rates along with extended response times lead to accelerated approvals. If the study of trastuzumab deruxtecan excludes prior ADC therapy, it will likely need to be routinely approved in a randomized trial comparing it with trastuzumab emtansines.
Find the right dose
MTDs are usually derived from safety data from phase 1 trials. But in fact, the cumulative toxicity of the drug will only appear after several courses of treatment, some of which will become more and more serious. For example, some promising ADCs have been associated with life-threatening pneumonia that occurs only after multiple cycles. Therefore, the recommended dose should be determined after careful analysis of multiple patients, multiple courses of treatment, and dose reductions and delays. It is much better to spend some extra time in the first phase perfecting the recommended dose than to have to go back and then publicly announce that the dose was reduced in the study.
Furthermore, the problem with many clinical trials is that the principal investigator is only nominal and patients are evaluated by a series of investigators, residents, and associate investigators. These individuals may have varying degrees of familiarity with the Common Toxicity Criteria ( NCI CTCs ). Staff caring for patients often did not consult the specific definitions associated with grades of toxicity, but instead used a common arbitrary description of mild (grade 1 ), moderate ( grade 2 ), severe ( grade 3 ) and life-threatening ( Grade 4 ) to describe toxicity other than hematologic and chemical profiles. This may lead to underreporting of drug toxicity, especially non-hematologic toxicity. Having investigators who are intimately familiar with NCI CTCs and have extensive experience with toxicity classification is key to accurate collection of safety data and successful determination of recommended dosing.
Finally, there is evidence that toxicity occurs repeatedly due to weight-based dosing. The vast majority of ADCs are dosed in mg/kg or mg/m2, yet there is little scientific evidence for this in oncology, let alone ADCs. Basic pharmacology tells us that antibodies or other macromolecular therapeutics are initially restricted to the vascular compartment. However, because adipose tissue is not well vascularized, vessel volume does not increase proportionally to total body weight. Weight-based dose escalation in obese or overweight patients would disproportionately increase plasma concentrations, resulting in increased toxicity. With obesity increasing in the Western world, this is a reality for research subjects and must be taken into account in clinical trials. In addition, some patients may develop third cavity effusions (ascites, edema, and pleural effusion).
In this regard, mirvetuximab soravtansine is a good example. During early clinical development of the drug, dose-limiting keratitis was a non-targeted oncological adverse event that occurred more frequently at higher doses when the drug was dosed at mg/kg. Despite numerous efforts, this corneal toxicity cannot be alleviated by topical measures such as lubrication or steroid eye drops. This poses a challenge to the feasibility of later development. Subsequently, the investigators performed detailed pharmacokinetic analysis and modeling to determine the relationship between Cmax and keratitis severity. Further studies demonstrated that dosing using the adjusted ideal body weight formula ( AIBW ) is required to achieve a safe and effective plasma concentration range in a series of patients. This method of delivery was further validated in a broader ovarian cancer patient population, with a significant reduction in keratitis from 40% to 10% while maintaining antitumor activity.
Since the therapeutic index of some ADCs is smaller than that of non-ADC antibody treatments, the relationship between dose, dose formula, clinical pharmacokinetics, and toxicity should be carefully analyzed and the optimal dosing approach should be determined.

Explore Multiple Dosing Options
Typically, only one dosing regimen is selected for phase 1 studies of ADCs . The usual dosing schedule for new agents is usually derived from cytotoxic agents, chosen every 3 weeks because this will approximate the time of hematologic recovery. In the antibody era, dosing is increasingly based on expected clearance and half-life, resulting in a dosing schedule every 2 to 4 weeks. Therefore, for ADC drugs, there is no reason to adopt the schedule of cytotoxic drugs or antibodies. Perhaps a better option is to select a schedule based on tolerability, pharmacokinetics, and / or kinetics of target antigen switching and target antigen regeneration.
Gemtuzumab ozogamicin ( Myelotarg® ) is an excellent case study in ADC development. Gemtuzumab ozogamicin, the first ADC drug approved by the FDA, was approved in 2000, followed by a voluntary withdrawal in 2010 and then reapproved in 2017. The initial schedule for this ADC is 9 mg/m2 every 2 weeks. In the earliest studies, a saturating pharmacokinetic pattern with a nonlinear dose-to-plasma concentration relationship was observed due to a disproportionate increase in drug concentration in plasma above CD33+ saturation levels. Accumulation of this drug in plasma, above the level necessary to saturate CD33+ target cells, is at least in part responsible for many of the toxicities observed, including myelosuppression, acute hepatotoxicity, and hepatic veno-occlusive disease after transplantation disease. In 2010, Gemtuzumab ozogamicin was voluntarily withdrawn from the market after subsequent confirmatory trials failed to verify its clinical efficacy and prove its safety.
Later studies established that the kinetics of CD33 expression switching on AML target cells is approximately every 3-4 days. Subsequently, the investigators provided a new regimen of administering a low dose of 3 mg/m2 every 3 days for 3 doses. Use a split dosing regimen to reduce peak and total plasma concentrations of gemtuzumab ozogamicin to within the expected dose-proportional range. Clinically, this resulted in greater tolerability and antitumor activity, and in 2017, the FDA reapproved Gemtuzumab ozogamicin.
Biomarker Strategies
The overarching strategy for ADC biomarker development is to identify and select the subset of cancer patients most likely to respond to ADCs , thereby achieving high rates of and durable responses, ensuring regulatory approval. The strategy to achieve this is often the biggest question in biomarker development.
In early studies, accept patients with tumors likely to express the target whenever possible
This may seem counterintuitive for the overall strategy just described, but it is one of the most common mistakes in early development and can significantly slow down clinical execution. To better understand the pre-screening issues for the presence of target antigens, it is essential to understand the actual process of tissue collection and analysis in clinical research.
Many patients do not have easily accessible archived tissue. And to obtain tissue for trial screening is a lengthy process, with even the fastest turnaround time for analysis still typically requiring six weeks for results. Now imagine that a patient has an advanced malignancy that has not responded to standard treatments and is being considered for a clinical trial. Will they wait for the pre-screening results? Or will they run another clinical trial that doesn’t require pre-screening? The answer is obvious to most and is reflected in the way clinical trial centers access patients.
Don’t wait until the assay is perfect
Biomarker development is complex. Although ADCs have antibodies as backbones, antibodies chosen for therapy may not perform satisfactorily for immunohistochemistry ( IHC ).
It is very common to select different antibody candidates for IHC biomarkers. The general recommendation is that concurrent clinical trials and biomarker development are often most effective.
Don’t be superstitious about the expression level of the target antigen
It must be admitted that tumor cells must target antigens in order to exert the anti-tumor activity of ADC. However, even high expression does not necessarily guarantee antitumor activity, and low expression does not necessarily guarantee no activity. The failure of ADCs to cause tumor cell death may be due to many factors independent of tumor cell expression.
Counterintuitively, responses were observed in some patients with low expression of the target antigen at initial diagnosis. This may be due to the age, quality, and specificity of the assay of the tissue sample, or due to increased expression of the target antigen as the disease progresses. Therefore, the most logical approach in early development is to select patients not solely on the basis of demonstrated target antigen expression in early clinical trials, but also to use data from the expansion phase to determine the relationship between expression and response.
Furthermore, not every ADC requires a biomarker for patient selection. For many hematological malignancies, the target cell is a specific lineage, so ADCs can target both normal and malignant cells, examples of which include CD33+, CD22, CD79b, and CD30.
Finally, if a biomarker unnecessarily or arbitrarily deprives patients of potentially beneficial treatments, this may limit commercial opportunities later on.
Do not change assay or cutoff parameters during the study
This may sound self-evident, but recent experience suggests otherwise. A recent example of this error is mirvetuximab soravtansine, an ADC targeting folate receptor alpha (FRa) in platinum-refractory ovarian cancer. In a phase II study, promising antitumor activity was observed in platinum-refractory ovarian cancer using selection criteria favoring high expression of FRa.
Unfortunately, however, the patient selection parameters tested were changed in the study, which included patients with intermediate FRa expression. This resulted in the primary endpoint of improvement in progression-free survival (PFS) not being met. Post hoc analysis found that the subset of patients with high expression (FRa) was as statistically significant as those in the earlier study.
Standard Clinical Pharmacology Considerations for ADCs
Until recently, many of the clinical pharmacology steps required for regulatory approval during ADC development were not outlined separately from the drug or biologic, raising the question, should ADCs be considered cytotoxic drugs, or are they closer to antibodies? This uncertainty has led to questioning the need for organ dysfunction studies, drug interaction studies, and comprehensive QTc studies.
Recently, FDA’s Center for Drug Evaluation and Research ( CDER ) and Center for Biologics Evaluation and Research ( CBER ) jointly released draft guidance to assist in the clinical development of ADCs. These very practical recommendations should help industry researchers determine what clinical pharmacology studies are needed. It can also be argued that the release of the guidelines further demonstrates that ADCs are a platform in their own right, beyond cytotoxicity and antibody development.
Summary
Currently, more than 20 new ADC drugs are in the early stage of development, and more are in the late stage of preclinical research.
The prospect of ADC therapy to improve cancer patients is very promising. The key to success is often learning from others and avoiding their mistakes.
It is hoped that this article can provide some useful and practical ways to ensure the success of clinical development that more closely mirrors the patient population, and that these lessons will provide the best path forward.
references:
1. Antibody drug conjugates: The dos and don’ts in clinical development. Pharmacol Ther. 2022 Jun 20;240:108235.
What have we learned from ADC (Antibody-drug conjugate) development?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.