Long-term Antibiotic Use: 36% Decreased Risk of Liver Cancer
- Brief Intermittent Exercise Reduces Heart Disease and Death Risk
- Personalized Lung Tumor Chips Assess PD-1 Therapy Response
- Study Shows Prior Infection Offers Strong Immunity to Original COVID-19 Strain
- Chinese Food Products Dominate Korean Tables Amid Safety Concerns
- Early Detection of Hypopharyngeal Cancer Possible with Saliva Diagnosis
- EB Virus Could Be Infected by Kiss: A Hidden Threat Linked to Cancer
Long-term Antibiotic Use: 36% Decreased Risk of Liver Cancer
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
“Cancer Communications”: Long-term Antibiotic Use Associated with a 36% Decreased Risk of Liver Cancer.
While most cancer research data suggests that antibiotic use can affect the efficacy of immune checkpoint inhibitors, liver cancer may be an exception.
Previously, it was reported that early antibiotic use significantly extended the progression-free survival of liver cancer patients receiving immune checkpoint inhibitor therapy.
Furthermore, early animal experiments indicated that the antibiotic tigecycline not only inhibited the proliferation of liver cancer cells in vitro but also induced apoptosis in liver cancer cells.
This suggests that antibiotics might have unexpected benefits in the context of liver cancer.
However, the relationship between antibiotic use and the progression of liver cancer has not been fully understood until now.
Recently, a study conducted by Sang Min Park’s team at Seoul National University Hospital in South Korea analyzed data from over 9.8 million participants aged ≥20.
They found that long-term antibiotic use (≥365 days) was associated with a 36% reduced risk of developing liver cancer compared to participants who had never used antibiotics (adjusted HR=0.64).
The study was published in the form of a letter in “Cancer Communications.”
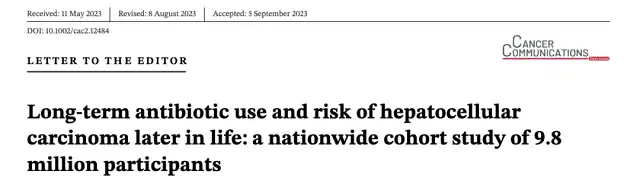
To investigate the relationship between antibiotic use and the risk of liver cancer development, researchers conducted a nationwide cohort study, ultimately selecting 9,805,027 participants aged ≥20 who had not been diagnosed with any cancer between 2005 and 2006. They collected health screening results, hospital and outpatient medical records, and prescription information from the Korean National Health Insurance Service (NHIS) database.
Follow-up began on January 1, 2007, and continued until the occurrence of liver cancer, death, or the end of the study on December 31, 2021. The cumulative days of antibiotic prescription in the five years before participants’ enrollment were used to determine antibiotic use, categorized as 0 days, 1-14 days, 15-59 days, 60-179 days, 180-364 days, and ≥365 days.
The results showed that the longer the duration of antibiotic use, the lower the risk of developing liver cancer. Specifically, after adjusting for age, gender, body mass index, cholesterol levels, Charlson comorbidity index, and chronic liver disease, long-term antibiotic use (≥365 days) was associated with a 36% reduced risk of liver cancer. Additionally, both men and women who used antibiotics long-term had a lower risk of liver cancer (adjusted HR for men=0.62; adjusted HR for women=0.73).
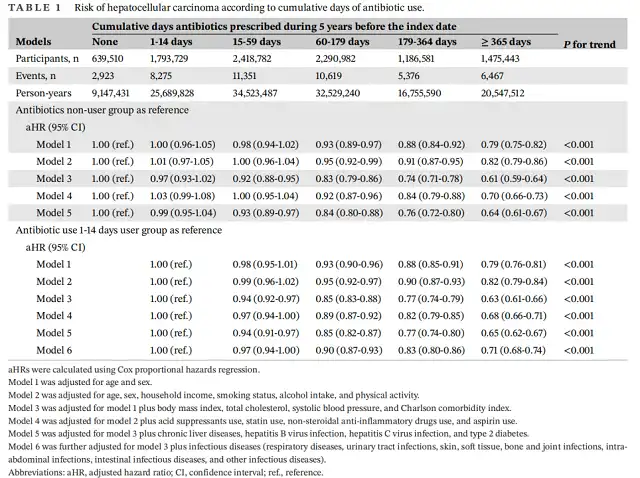
Relationship between cumulative days of antibiotic prescription and risk of liver cancer
Further sensitivity analysis indicated that even after excluding participants with factors related to an increased risk of liver cancer (such as pre-existing chronic liver disease, hepatitis B virus [HBV] infection, and type 2 diabetes), long-term antibiotic use was still associated with a reduced risk of liver cancer (HR=0.70).
Moreover, the researchers evaluated the relationship between the types of antibiotics used and the risk of liver cancer development. The results showed that using five or more different types of antibiotics was associated with a 35% reduced risk of liver cancer compared to participants who had never used antibiotics (adjusted HR=0.65).
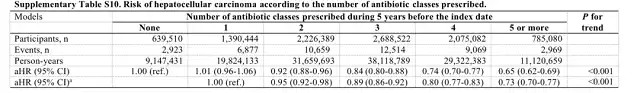
The relationship between the types of antibiotics taken and the risk of liver cancer
In summary, in this nationwide cohort study, researchers found an association between the cumulative days of antibiotic prescription and a reduced risk of liver cancer. The longer the duration of antibiotic use, the lower the risk of developing liver cancer.
Traditionally, antibiotics have been viewed as having negative effects, including disrupting the gut microbiome and increasing the risk of certain diseases like cardiovascular disease, as well as potentially affecting the efficacy of immune checkpoint inhibitors. However, the authors of this study noted that antibiotics like tigecycline and amikacin may inhibit liver cancer development by lowering deoxycholic acid levels in mouse liver tissue, which could be one of the reasons for the decreased risk of liver cancer associated with antibiotic use.
Of course, the authors also emphasized that the cumulative days of antibiotic prescription may not represent the actual dosage of antibiotics taken, and further research with larger sample sizes and data from more regions will be needed to validate these findings. Let’s look forward to future developments in this area!
Reference:
[1] Jeong S, Park SJ, Kim M, Park YJ, Choi S, Chang J, Kim JS, Oh YH, Ko A, Park SM. Long-term antibiotic use and risk of hepatocellular carcinoma later in life: a nationwide cohort study of 9.8 million participants. Cancer Commun (Lond). 2023 Sep 13.
Long-term Antibiotic Use: 36% Decreased Risk of Liver Cancer
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.