Major Reversal: Supplementing Vitamin D Doesn’t Work!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Major Reversal: Supplementing Vitamin D Doesn’t Work!
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Major Reversal: Supplementing Vitamin D Doesn’t Work!
In a surprising turn of events, the latest publication in The Lancet reveals that supplementing Vitamin D cannot reduce the risk of death and the incidence of cardiovascular diseases, according to data from a study involving over 500,000 individuals.
As cold air sweeps in and temperatures take a plunge, the winter chill intensifies. The time available for basking in the sun diminishes, making sunlight increasingly precious. With the onset of winter, a noticeable change occurs: a widespread deficiency of Vitamin D.
Vitamin D, a crucial fat-soluble vitamin for maintaining life, is synthesized either through exposure to ultraviolet rays on the skin or obtained from diet and supplements. Data shows that 80% of Vitamin D in the body is synthesized in the skin after exposure to sunlight, earning it the nickname “sunshine vitamin.”
However, with winter’s arrival, the time people spend in the sun decreases, coupled with dietary neglect of Vitamin D intake, making Vitamin D deficiency and insufficiency a significant public health issue in China and globally. The “2015-2017 China Resident Nutrition and Health Status Monitoring Report” indicates a 21.4% deficiency rate in serum Vitamin D levels among Chinese adults aged 18 and above. Globally, around 30-60% of children and adults are reported to have insufficient levels of Vitamin D.
Vitamin D deficiency doesn’t show immediate effects, and many individuals may not even be aware of their “deficient state.” Inadequate Vitamin D levels can impact health in various ways, including bone health, muscle strength, autoimmune diseases, type 2 diabetes, and more.
For the sake of health, should one consider supplementing Vitamin D at this time?
Two years ago, the largest-scale study at the time, involving multiple teams such as the Prospective Studies of Nutrition Cardiovascular Diseases (EPIC-CVD) and the Vitamin D Studies Collaboration (VitDSC), published in The Lancet suggested that Vitamin D deficiency is widespread and closely linked to health.
Observational analysis indicated that low concentrations of 25(OH)D in the blood are associated with increased risks of coronary heart disease, stroke, and overall mortality. Furthermore, the researchers conducted a Mendelian randomization analysis on a subset of the population, revealing a causal relationship between serum 25(OH)D levels and mortality for those deficient in Vitamin D.
This study led to increased interest in Vitamin D supplements.
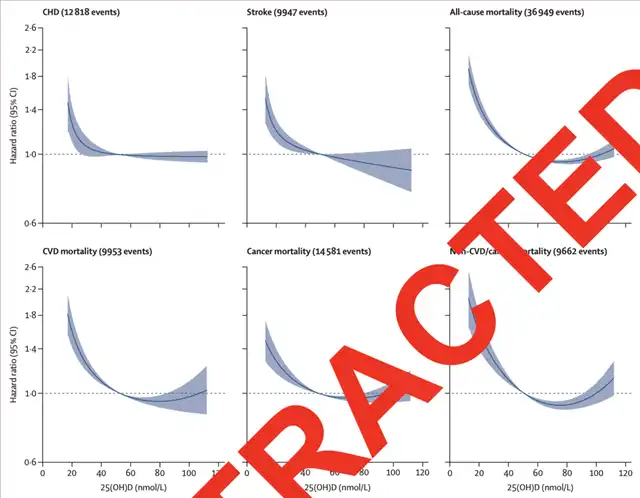
Association between serum 25(OH)D levels and various diseases
Contrary to expectations, after some scholars questioned the effectiveness of the statistical methods used in the study and raised concerns about the results from Mendelian randomization analysis, the research team reanalyzed the data and came up with a “shocking reversal”!
The latest analysis and revised findings indicate that there is no causal relationship between serum 25(OH)D levels and the outcomes of cardiovascular disease and mortality, whether or not there is a deficiency in Vitamin D. Even for individuals deficient in Vitamin D, long-term low-dose supplementation cannot significantly reduce mortality and the incidence of cardiovascular diseases.
It seems that supplementing Vitamin D is truly “futile”!
DOI:https://doi.org/10.1016/S2213-8587(23)00287-5
In this study, the researchers conducted the largest observational analysis to date, observing and analyzing data from 31 studies involving a total of 500,962 participants from the UK Biobank, EPIC-CVD, and VitDSC collaborations, including 384,711 from the UK Biobank, 26,336 from EPIC-CVD, and 67,992 from VitDSC.
The observational analysis revealed a “non-linear shape” of the correlation. Specifically, when serum 25(OH)D concentrations are low, the correlation is inversely proportional to all outcomes. However, when 25(OH)D concentrations are high, there is no association with cardiovascular disease-related mortality, and the correlation with other mortality outcomes is weakly positive.
For example, in cases of coronary heart disease and stroke, when serum 25(OH)D concentrations are above 50nmol/L, there is almost no correlation between Vitamin D and the incidence rates of coronary heart disease and stroke. In other words, even if blood Vitamin D levels are high, it does not significantly reduce the risk of disease occurrence. However, when serum 25(OH)D concentrations are below the critical level, the correlation gradually strengthens.
To more accurately assess the potential causal relationship between Vitamin D supplements and health, the researchers further used Mendelian randomization, a method based on genetic variation for causal inference. Unlike traditional observational analysis, Mendelian randomization analysis provides more reliable causal relationships.
Genetic analysis data came from the UK database, EPIC-CVD, and two Copenhagen population studies, including 333,002 participants from the UK Biobank with 25(OH)D measurement levels and genetic data, as well as 22,142 from EPIC-CVD, 31,262 from the Copenhagen City Heart Study (CCHS), and the Copenhagen General Population Study (CGPS).
In the end, among the 386,406 participants included in the genetic analysis, which included 33,546 coronary heart disease patients and 18,166 stroke patients, 27,885 deaths were recorded.
Contrary to the results of observational analysis, overall Mendelian randomization analysis showed no association between genetically predicted 25(OH)D levels and the incidence rates of coronary heart disease, stroke, and overall mortality. However, in the Copenhagen study, there was some evidence suggesting an inverse relationship between 25(OH)D and overall mortality (p=0.03).
In summary, regardless of whether observational analysis shows a critical relationship between serum 25(OH)D levels and cardiovascular diseases and mortality risks, genetic analysis fails to prove this point. In other words, supplementing Vitamin D in cases of deficiency is unlikely to reverse the risks.
Major Reversal: Supplementing Vitamin D Doesn’t Work!
References:
[1]Emerging Risk Factors Collaboration/EPIC-CVD/Vitamin D Studies Collaboration. Estimating dose-response relationships for vitamin D with coronary heart disease, stroke, and all-cause mortality: observational and Mendelian randomisation analyses. Lancet Diabetes Endocrinol. 2021 Dec;9(12):837-846. doi: 10.1016/S2213-8587(21)00263-1. Epub 2021 Oct 28. Erratum in: Lancet Diabetes Endocrinol. 2023 Dec 1;: PMID: 34717822; PMCID: PMC8600124.
Emerging Risk Factors Collaboration/EPIC-CVD/Vitamin D Studies Collaboration. Estimating dose-response relationships for vitamin D with coronary heart disease, stroke, and all-cause mortality: observational and Mendelian randomisation analyses. Lancet Diabetes Endocrinol. 2023 Dec 1:S2213-8587(23)00287-5. doi: 10.1016/S2213-8587(23)00287-5. Epub ahead of print. PMID: 38048800.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



