Study confirmed the causal relationship between vitamin D deficiency and death
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Study confirmed the causal relationship between vitamin D deficiency and death
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Study confirmed the causal relationship between vitamin D deficiency and death.
Sub-Journal of The Lancet: Vitamin D deficiency is not a small problem! The largest study to date has confirmed that there is a causal relationship between vitamin D deficiency and death丨Clinical discovery
Friends with low levels of vitamin D in the body, you may have to take vitamin D supplementation seriously.
Recently, the Dr. Stephen Burgess research team from the Biostatistics Unit of the Medical Research Council of the University of Cambridge published an important result of a vitamin D-related study in the journal “The Lancet Diabetes and Endocrinology” [1].
They conducted a pooled analysis of data from 33 prospective studies. The results of this observational study suggest that the low concentration of the vitamin D metabolite 25 hydroxyvitamin D (25[OH]D) in the blood is associated with coronary heart disease, stroke, and all patients. It is related to an increased risk of death.
Mendelian randomization studies have shown that in people with vitamin D deficiency (25[OH]D concentration <25 nmol/L), the genetically predicted 25[OH]D concentration increases by 10 nmol/L, the risk of all-cause death is reduced 31% .
More detailed grouping analysis suggests that the reverse causal relationship between the two is established within the range of 25[OH]D <40 nmol/L predicted by genetics.
The significance of this study is that it was the first to find evidence of a genetic causal association between 25[OH]D concentration and all-cause death in groups with low vitamin D levels .
It can be used to inspire and improve the design of future vitamin D supplementation trials, and provide ideas and references for prevention strategies for related diseases.
Article title map
Vitamin D is an essential part of the regulation of calcium and phosphorus metabolism in the human body. Previous observational studies have suggested that vitamin D deficiency is related to the occurrence of cardiovascular diseases and the increased risk of all-cause death [2-3].
But the strange thing is that these associations have not been reflected in randomized controlled trials of vitamin D supplements [4].
Some researchers speculate that this phenomenon may be due to the fact that most randomized controlled trials did not take into account the subjects’ baseline vitamin D levels [5].
However, it is not clear what is the difference between 25[OH]D and clinical events at different blood concentrations.
The Mendelian randomization method uses the Mendelian inheritance law of “parental alleles are randomly assigned to offspring”, and genotype is used as a tool variable to analyze the association between exposure factors and diseases, which is a powerful tool for inferring potential causal associations.
The conclusions of previous Mendelian randomization studies on vitamin D are also divergent [6-7], and previous studies have assumed a linear dose-response relationship between 25[OH]D and clinical events predicted by genetics, which is not consistent with observational studies.
Found a non-linear trend [8], this inaccurate assumption may affect the accuracy of the conclusion.
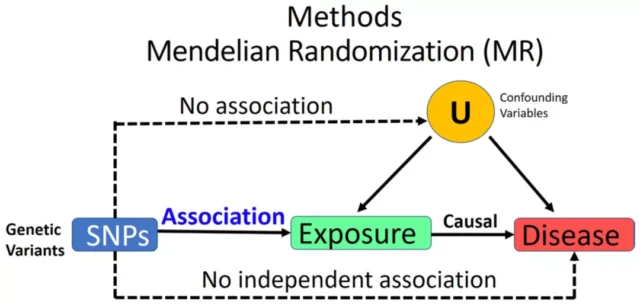
Illustration of Mendelian randomization method [9]
In order to more accurately analyze the association between vitamin D concentration and cardiovascular events, stroke, all-cause death and other outcomes, the Stephen Burgess research team carried out the largest meta-analysis of individual-level data so far , and carried out stratified Mendelian randomization.
Chemical research to clarify the possible causal relationship between 25[OH]D concentration and clinical events.
Stephen Burgess team used data from UK Biobank, European Prospective Investigation of Cardiovascular Diseases in Cancer and Nutrition (EPIC-CVD), Vitamin D Research Collaboration Group (VitDSC), Copenhagen Population Study and other sources.
These study groups have a median follow-up time ranging from 8.8 to 21.4 years . The observational analysis included 500,962 participants, and the Mendelian study included 386,406 participants.
The main outcomes include coronary heart disease, stroke, and death from all causes.
The researchers used inverse variance weighted random effects meta-analysis to combine the hazard ratios of different studies, considering the genetic variation of four gene regions closely related to 25[OH]D and related to the transportation, metabolism and synthesis of vitamin D, and used stepwise Method screening.
The genetic risk score was calculated based on the conditional association of the genetic variation of the 25[OH]D concentration in the UK Biobank.
Use Logistic regression/linear regression to estimate genetic associations. In addition to the overall population, this study also analyzed the causal association under different residual 25[OH]D concentration stratification.
Observational research results suggest that low concentrations of 25[OH]D are significantly associated with increased risks of coronary heart disease, stroke, all-cause death, cardiovascular death, tumor death, non-cardiovascular and tumor death .
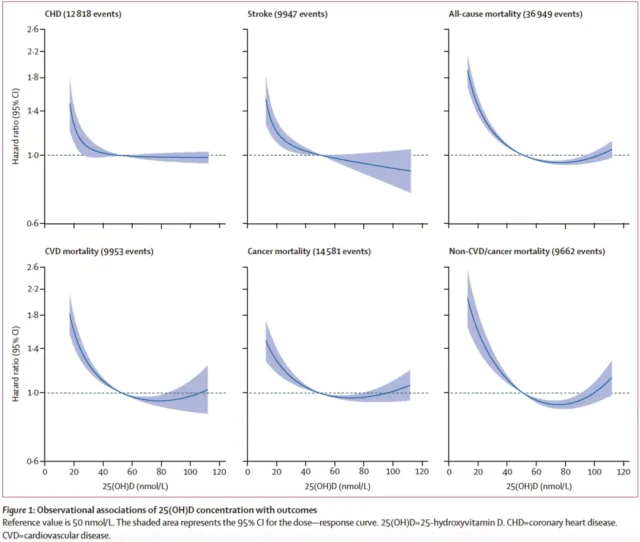
25[OH]D and Outcome Observational Research Results
Mendelian randomization analysis results show that after stratifying 25[OH]D according to residual concentration, vitamin D deficiency (25[OH]D<25 nmol/L) and all-cause mortality have significant reverse causality Associated .
For every 10 nmol/L increase in 25[OH]D concentration predicted by genetics, the risk of death from all causes decreased by 31% (odds ratio: 0.69, P<0.0001) .
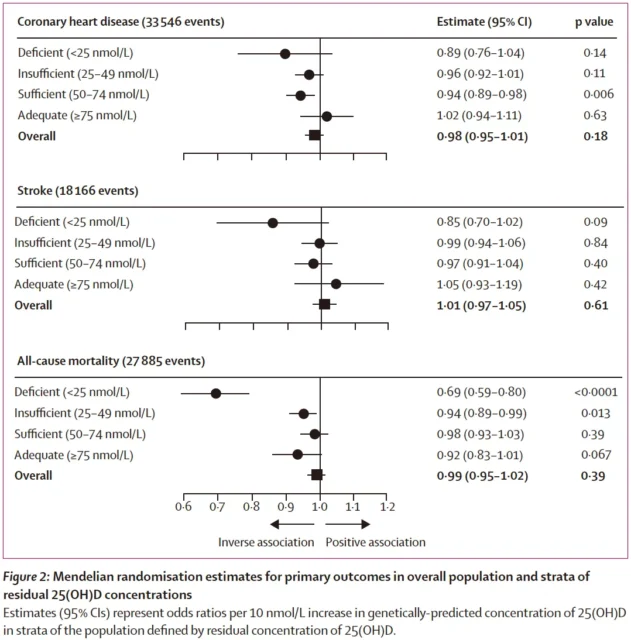
Results of Mendelian Randomization Analysis of 25[OH]D and Primary Outcomes
This association is also statistically significant when cardiovascular mortality, non-cardiovascular disease and tumor mortality are the outcomes.
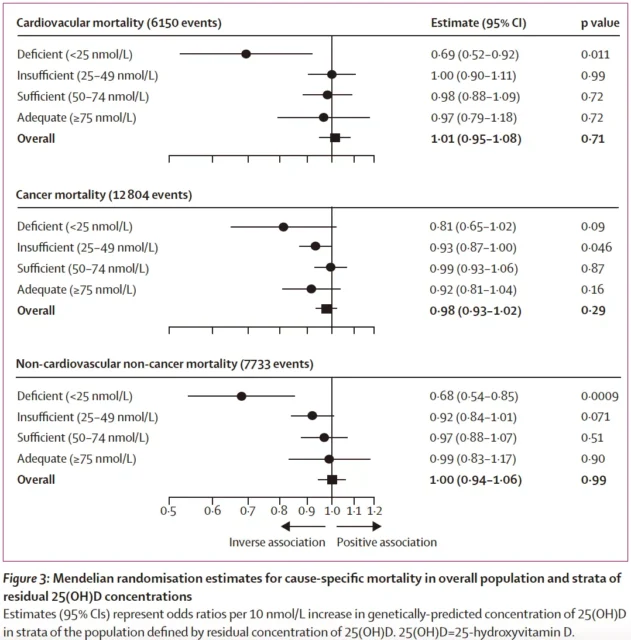
Mendelian randomization analysis results of 25[OH]D and other clinical outcomes
A more detailed grouping analysis suggests that the genetically predicted increase in 25[OH]D concentration and the reduced risk of all-cause death are inversely causally related, both within the range of residual 25[OH]D concentration <40 nmol/L .
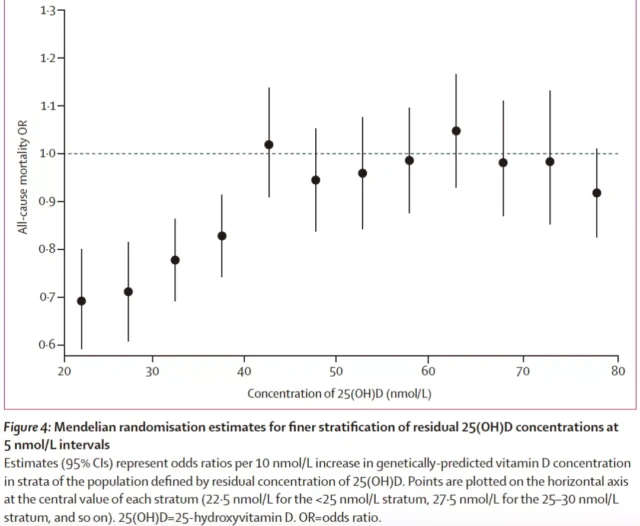
Results of a more refined Mendelian randomization study
It is worth mentioning that this study used data from more than 500,000 people and combined a variety of statistical methods to ensure the reliability of the conclusions.
In addition, Mendelian randomization avoids the possibility of causal inversion and reduces the influence of confounding factors.
Of course, this study also has certain limitations. For example, instrumental variables related to vitamin D may not be the best choice. In some studies, genetic data is relatively small, which limits the use of data to a certain extent. In addition, the relatively single ethnic composition of this study may also limit the promotion of future results.
In general, this study found the possible reasons for the repeated failure of RCTs in the past through the stratified analysis of the 25[OH]D levels of the participants: the effect of vitamin D supplementation on subjects with different baseline 25[OH]D levels big different.
For those with low baseline vitamin D levels, vitamin D supplements may have some value.
This study also reminds clinicians that when analyzing and intervening adverse clinical outcomes such as all-cause death, cardiovascular death, and stroke, they may also consider causal factors such as vitamin D as targets.
Perhaps in some specific populations, simple nutritional supplements or lifestyle interventions are far stronger than the effects of drugs and surgery in the long run.
This study and similar studies in the future may provide new ideas and basis for clinical disease intervention.
references
[1] Emerging Risk Factors Collaboration/EPIC-CVD/Vitamin D Studies Collaboration. Estimating dose-response relationships for vitamin D with coronary heart disease, stroke, and all-cause mortality: observational and Mendelian randomisation analyses. Lancet Diabetes Endocrinol. 2021; S2213-8587(21)00263-1. doi:10.1016/S2213-8587(21)00263-1
[2] Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503-511. doi:10.1161/CIRCULATIONAHA.107.706127
[3] Heath AK, Kim IY, Hodge AM, English DR, Muller DC. Vitamin D Status and Mortality: A Systematic Review of Observational Studies. Int J Environ Res Public Health. 2019;16(3):383. Published 2019 Jan 29. doi:10.3390/ijerph16030383
[4] Manson JE, Cook NR, Lee IM, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. 2019;380(1):33-44. doi:10.1056/NEJMoa1809944
[5] Zhang Y, Fang F, Tang J, et al. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ. 2019;366:l4673. Published 2019 Aug 12. doi:10.1136/bmj.l4673
[6] Brøndum-Jacobsen P, Benn M, Afzal S, Nordestgaard BG. No evidence that genetically reduced 25-hydroxyvitamin D is associated with increased risk of ischaemic heart disease or myocardial infarction: a Mendelian randomization study. Int J Epidemiol. 2015; 44(2):651-661. doi:10.1093/ije/dyv078
[7] Afzal S, Brøndum-Jacobsen P, Bojesen SE, Nordestgaard BG. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. BMJ. 2014;349:g6330. 2014 Nov 18. doi:10.1136 /bmj.g6330
[8] Zhang R, Li B, Gao X, et al. Serum 25-hydroxyvitamin D and the risk of cardiovascular disease: dose-response meta-analysis of prospective studies. Am J Clin Nutr. 2017;105(4):810 -819. doi:10.3945/ajcn.116.140392
[9] Soliman GA, Schooling CM. Causal association between mTOR-dependent EIF-4E and EIF-4A circulating protein levels and type 2 diabetes: a Mendelian randomization study. Sci Rep. 2020;10(1):15737. Published 2020 Sep 25. doi:10.1038/s41598-020-71987-8
Study confirmed the causal relationship between vitamin D deficiency and death.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



