Vitamin D Supplementation Fails to Lower Death and Cardiovascular Risk Long-Term
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Surprising Reversal: Vitamin D Supplementation Fails to Lower Death and Cardiovascular Risk Long-Term
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Surprising Reversal: Vitamin D Supplementation Fails to Lower Death and Cardiovascular Risk Long-Term
Analysis of over 800,000 individuals’ data shows that long-term, low-dose vitamin D supplementation is unlikely to reduce the risk of death and cardiovascular disease, even in individuals with insufficient vitamin D levels.
Two years ago, the journal “The Lancet Diabetes & Endocrinology” published a study, the largest at that time, reminding us of the importance of supplementing vitamin D.
In this study, an observational analysis of data from over 500,000 individuals in 33 prospective studies found that lower concentrations of the vitamin D metabolite 25-hydroxyvitamin D (25[OH]D) in the blood were associated with an increased risk of coronary heart disease, stroke, and all-cause mortality.
Subsequent Mendelian randomization analysis in over 380,000 individuals further indicated a genetic causation between 25[OH]D levels and all-cause mortality in populations with vitamin D deficiency, suggesting the importance of vitamin D supplementation in reducing the risk of death.
However, there has been a major reversal in this paper recently.
After some scholars raised concerns about the assumptions in the model used in the Mendelian analysis, the research team reanalyzed the data and arrived at conclusions completely opposite to those before.
Regardless of whether there is a lack of vitamin D, there is no causal relationship between 25[OH]D concentration and death or cardiovascular disease. This indicates that even for individuals deficient in vitamin D, long-term, low-dose vitamin D supplementation is unlikely to significantly reduce the risk of death and cardiovascular disease.
It can be understood that individuals with insufficient vitamin D may have a higher risk of cardiovascular disease and all-cause mortality, but these risks are likely not due to vitamin D deficiency, and supplementing vitamin D cannot reverse the risks.

Vitamin D is an essential nutrient for the human body, and observational epidemiological studies consistently associate low levels of circulating 25[OH]D with an increased risk of cardiovascular disease, all-cause mortality, and other chronic diseases.
Contrary to this, several large randomized trials on vitamin D supplementation have failed to conclude that supplementing vitamin D can reduce the risk of disease and death.
Mendelian analysis uses genetic information as a tool variable to analyze the association between exposure factors and disease, serving as a powerful tool for inferring potential causal relationships.
In the previously retracted paper, researchers erroneously assumed a linear relationship between genetically predicted 25[OH]D levels and the reaction to cardiovascular disease, using a residual method, which does not reflect the actual situation.
Mendelian analysis data come from four large cohorts, including the UK Biobank, the European Prospective Investigation into Cancer and Nutrition Cardiovascular Disease study (EPIC-CVD), the Vitamin D Study Collaboration (VitDSC), and the Copenhagen General Population Study, comprising 386,406 individuals of European descent.
In the overall analysis, genetically predicted 25[OH]D levels were unrelated to coronary heart disease, stroke, and all-cause mortality; the conclusion remained unchanged when stratified by 25[OH]D levels.
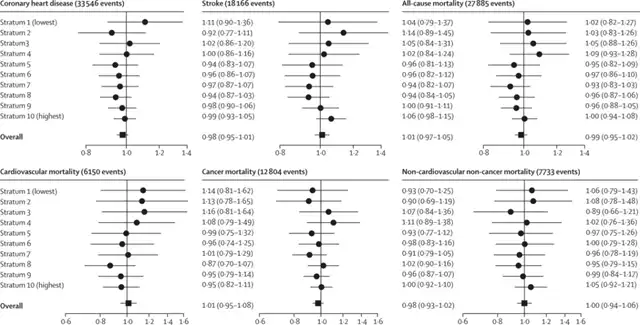
25[OH]D levels were not causally related to the primary outcome
However, previous observational analysis results still stand.
Observational analysis of data from 33 prospective studies and 500,926 participants found that the association curve between all outcomes and 25[OH]D levels is similar. In individuals with low 25[OH]D levels, there is an association with higher cardiovascular disease/death and all-cause mortality risk.
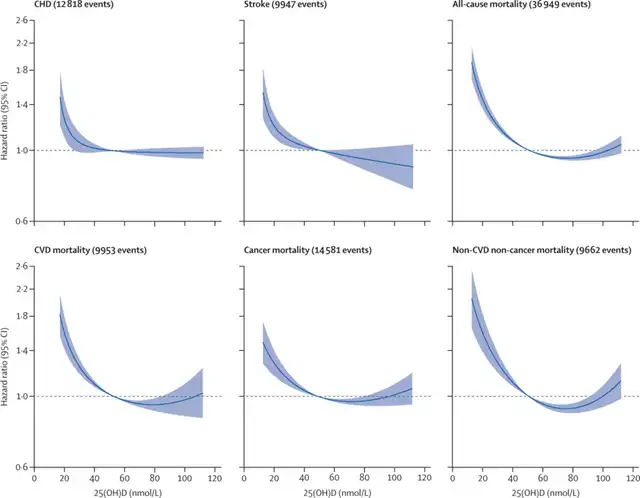
Low 25[OH]D levels linked to increased risk of disease/death
In summary, although observational analysis finds a certain correlation between 25[OH]D and cardiovascular disease and death, this has not been confirmed in genetic analysis. Even with low 25[OH]D levels, supplementing 25[OH]D has no causal impact on cardiovascular disease and death.
Surprising Reversal: Vitamin D Supplementation Fails to Lower Death and Cardiovascular Risk Long-Term
References:
[1]https://www.thelancet.com/journals/landia/article/PIIS2213-8587(23)00287-5/fulltext
[2]https://www.thelancet.com/journals/landia/article/PIIS2213-8587(23)00364-9/fulltext
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



