BMJ: Vitamin D supplementation can also improve immunity!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
BMJ: Vitamin D supplementation can also improve immunity! Large clinical trial shows that taking vitamin D can reduce risk of autoimmune disease by 22%
As an important supplement, the role of vitamin D in various aspects of prevention has always received much attention.
After studying both cancer and cardiovascular disease, the researchers turned their attention to autoimmune diseases.
Because 1,25-hydroxyvitamin D is a molecule known to regulate the expression of inflammatory genes, as well as the immune response [1].
Previous observational studies and small clinical trials have tested the effect of vitamin D in preventing disease progression in patients with established autoimmune diseases, but the results have been inconsistent, and in terms of prevention, no clinical trials have provided results.
In a recent BMJ, the results of a randomized, double-blind, placebo-controlled trial in more than 25,000 participants showed that taking vitamin D with or without added omega-3 fatty acids can reduce autoimmune disease The risk decreased by 22% [2].
A total of 25,871 participants were enrolled in the trial, who were required to supplement no more than 800 IU/day of vitamin D from external sources and were not taking fish oil supplements.
The experimental design is 2×2, divided into two groups and four groups. The two groups are the vitamin D group and the placebo group.
The vitamin D group is subdivided into two groups: “vitamin D3 + fish oil” and “vitamin D3 + placebo mimicking fish oil”.
The placebo group was subdivided into two groups: “placebo mimicking vitamin D + fish oil” and “placebo mimicking vitamin D + placebo mimicking fish oil”.
The dose of vitamin D was 2000 IU/day, and the omega-3 fatty acid was 1 g/day, and the median follow-up of the trial was 5.3 years.
The mean age of the participants was 67.1 years and included multiple races or ethnicities including non-Hispanic whites and blacks, and baseline characteristics between the four groups, such as annual income, education, serum 25-hydroxyvitamin D levels, exercise habits, BMI And family history of autoimmune disease, etc. are all balanced.
During follow-up, 123 people in the vitamin D group and 155 people in the placebo group were diagnosed with autoimmune disease, and after adjusting for multiple confounders, the vitamin D group had a 22% lower risk compared to the placebo group (p= 0.05).
When grouped by omega-3 fatty acids versus placebo, with 130 and 148 diagnosed autoimmune diseases, respectively, the omega-3 fatty acid group had a 15%, but not statistically significant, risk reduction (p =0.19).
Overall, however, the cumulative incidence was lower in both supplement groups than in the placebo group.
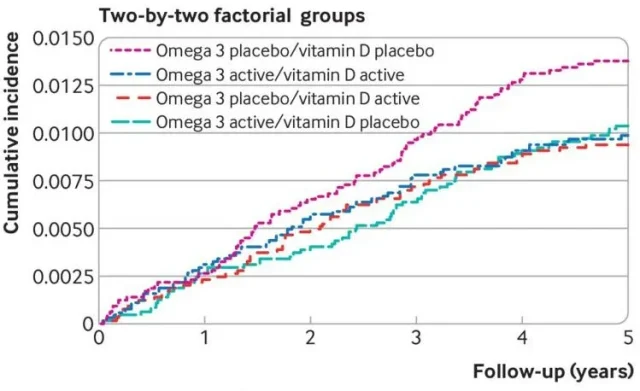
Cumulative incidence of vitamin D3 + fish oil (blue), vitamin D3 + placebo simulated fish oil (green), placebo simulated vitamin D + fish oil (red), and placebo simulated vitamin D + placebo simulated fish oil (purple)
After analyzing the participant data in four more detailed subgroups, the researchers again determined that the cumulative incidence was lower in all three supplement groups than in the double placebo group.
After adjustment for age, sex, and race, the risk of autoimmune disease was reduced by 31% (95% CI 0.49-0.96) in the dual supplement group and by 32% (95%) in the vitamin D + fish oil placebo group compared with the dual placebo group CI 0.48-0.94), the benefit of prevention was not significant for omega-3 fatty acids alone.
There was no significant interaction between the two supplements (p=0.20).
The researchers believe that there may be several potential mechanisms for the benefits of vitamin D in preventing autoimmune diseases.
The metabolite of vitamin D, 1,25-hydroxyvitamin D, binds to vitamin D receptors and regulates the expression of a series of genes, among them Including many involved in inflammation and immune response [3], vitamin D receptors are abundant on dendritic cells, T and B cells, and macrophages, so their function is affected by 1,25-hydroxyvitamin D. adjustment [4].
1,25-Hydroxyvitamin D inhibits the proinflammatory cytokine interleukin-6 (IL-6), an important factor in the activation of helper T cells17, which also secrete proinflammatory cytokines, are T cells known to be involved in the development of autoimmune diseases [5].
In addition, 1,25-hydroxyvitamin D can also inhibit the production of B-cell autoantibodies, promote the differentiation of monocytes into macrophages, inhibit pro-inflammatory cytokines and chemokines, and reduce major histocompatibility complex II by reducing the (MHC II) expression to reduce antigen-presenting ability [6].

However, the researchers suggest that the participants in this trial were on average older, a finding that may not hold in younger people, but that some autoimmune diseases, such as rheumatoid arthritis and psoriasis, have pathogenesis in older people. are similar in younger and younger patients and, therefore, may hold true in certain types of autoimmune disease.
Overall, this large clinical trial suggests that long-term vitamin D supplementation may reduce the risk of autoimmune disease.
The researchers said they will continue to follow participants for two years in an extension trial to observe the course of disease risk reduction over time, and in the future, the benefits of vitamin D will need to be tested in younger cohorts.
references:
[1] Kriegel MA, Manson JAE, Costenbader K H. Does vitamin D affect risk of developing autoimmune disease?: a systematic review[C]//Seminars in arthritis and rheumatism. WB Saunders, 2011, 40(6): 512- 531. e8.
[2] https://www.bmj.com/content/376/bmj-2021-066452
[3] Bouillon R, Marcocci C, Carmeliet G, et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions[J]. Endocrine reviews, 2019, 40(4): 1109-1151.
[4] Dankers W, Colin EM, van Hamburg JP, et al. Vitamin D in autoimmunity: molecular mechanisms and therapeutic potential[J]. Frontiers in immunology, 2017, 7: 697.
[5] Stockinger B. Th17 cells: an orphan with influence[J]. Immunology and cell biology, 2007, 85(2): 83.
[6] Linker-Israeli M, Elstner E, Klinenberg JR, et al. Vitamin D3 and its synthetic analogs inhibit the spontaneous in vitro immunoglobulin production by SLE-derived PBMC[J]. Clinical immunology, 2001, 99(1): 82 -93.
BMJ: Vitamin D supplementation can also improve immunity!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



