WHO Raises Attention Level for JN.1: Do We Need to Worry About COVID-19 Again?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
WHO Raises Attention Level for JN.1: Do We Need to Worry About COVID-19 Again?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
WHO Raises Attention Level for JN.1: Do We Need to Worry About COVID-19 Again?
The arrival, timing, and severity of JN.1, a new variant of concern, are influenced by multiple factors, introducing uncertainty. However, it is significantly distant from the peak observed a year ago.
On December 19, the World Health Organization (WHO) released a risk assessment report, adjusting the attention level for the new variant JN.1, categorizing it as a “variant of interest (VOI)” due to its significant transmission advantage.
As of December 16, at least 41 countries, including China, have reported the detection of JN.1, with a total of 7,344 virus gene sequences uploaded to the Global Initiative on Sharing Avian Influenza Data (GISAID). France, the United States, and Singapore lead in reported cases.
Noteworthy Spread and Potential Dominance in China:
JN.1 is a descendant branch of the Omicron variant BA.2.86, first detected on August 25 this year. WHO data indicates a continuous increase in its global infection rate. Currently, in the Americas, Europe, and the Western Pacific region, JN.1 is the fastest-spreading variant among circulating variants, with a prevalence of 65.6%, particularly reaching 72.7% in Singapore.
The prevalence of JN.1 in Singapore surged from 1.4% to 72.7%, while in France, it rose from 10.9% to 45.5%. On December 19, Singapore resumed daily reporting of infections. Concurrently, the country’s confirmed cases, after three weeks of continuous surge, began to decline from a daily peak of 7,870 to 6,530. Malaysia, a neighboring country, recorded nearly 27,000 cumulative cases from December 10 to 16, marking a 62.2% increase from the previous week. The health department in Malaysia reactivated the epidemic prevention app “MySejahtera” and continuously shared “isolation guidelines” on social media, urging confirmed cases to self-isolate for 5 days.
According to the U.S. Centers for Disease Control and Prevention (CDC) data as of December 8, JN.1 infections constitute approximately 15%-29% of new COVID-19 cases in the United States. During the same period, indicators of severity, such as COVID-19 hospitalizations, increased, while infection positivity rates and emergency room visits declined. By early December, wastewater monitoring in 22 U.S. states showed COVID-19 virus positivity rates reaching the CDC-defined “very high” level.
A virology expert told “Medicine” magazine, “Hospitalization rates are increasing overseas, not necessarily because JN.1 is more pathogenic, but due to an increase in the number of infections.”
“Countries that have been further from the previous COVID-19 infection peak experience a more significant decline in herd immunity, making them more susceptible to JN.1 invasion, including Singapore and the United States,” said the aforementioned virology expert. “China experienced its infection peak in mid-December last year, and many people had a second infection this year, maintaining a certain level of herd immunity. Based on overseas timelines, we need to be highly vigilant around the Chinese New Year. The arrival, timing, and severity of JN.1 are influenced by multiple factors, introducing uncertainty, but it is certainly far from the peak observed a year ago.”
On December 15, the National Health Commission of China published a popular science article stating that although the current prevalence of the JN.1 variant is extremely low in China, the possibility of JN.1 becoming the dominant variant domestically cannot be ruled out, influenced by international variants and imported cases.
Lu Hongzhou, the director of the National Infectious Diseases Clinical Medical Research Center, mentioned in an interview that the future prevalence of JN.1 in China might cause a small spike in infections, leading to a certain extent of increased burden on hospitals. However, our existing experience and medical resources are sufficient to handle this situation.
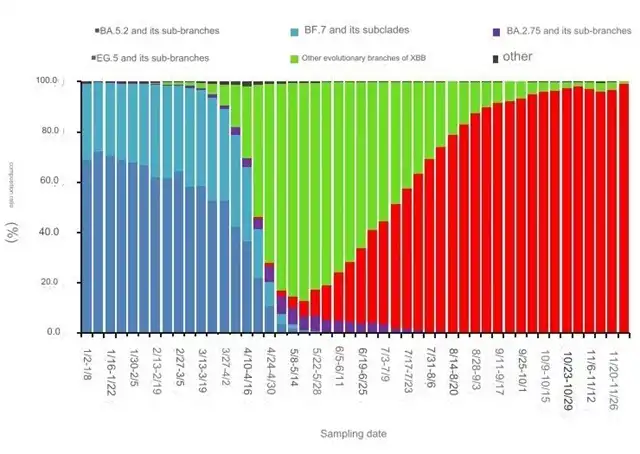 Trend of Variants in Local Cases of Novel Coronavirus Infection Nationwide. Source/China CDC
Trend of Variants in Local Cases of Novel Coronavirus Infection Nationwide. Source/China CDC
“Moderate” Threat, Milder Symptoms After Reinfection for Most:
Since March 15 this year, WHO has categorized variants based on their transmission and infection capabilities into three levels: “Variant Under Monitoring (VUM),” Variant of Interest (VOI), and “Variant of Concern (VOC).”
VOCs have strong transmission capabilities and high toxicity, significantly impacting the pandemic and posing the greatest global threat. The previously identified strains Alpha, Beta, Gamma, Delta, and the Omicron B.1.1.529 lineage fall into this category.
VOIs are confirmed to have community transmission cases globally or have been found in multiple countries but have not caused extensive spread or severe consequences. On November 21, JN.1, as a branch of the Omicron variant BA.2.86, was categorized as a VOI, along with other branches of the lineage.
According to the WHO report, JN.1 exhibits a high transmission growth advantage, but the risk of immune escape is “moderate,” and the risk of clinical severity after infection is “low.” Based on existing evidence, it is unlikely to significantly burden public health systems in various countries.
The virologist mentioned earlier stated that there is currently no evidence to suggest an increase in the transmission capability of JN.1. The greatest uncertainty lies in the potential further strengthening of immune escape by JN.1.
On December 15, a research team led by Cao Yunlong at Peking University published the latest study in “The Lancet Infectious Diseases,” finding that, compared to the currently dominant strains, BA.2.86 does not exhibit substantial fluid immune escape and growth advantage. However, its high affinity for the ACE2 receptor allows it to accumulate immune-evading mutations during periods of low-level community transmission.
JN.1 is an example of this. It quickly became the dominant strain in France, accumulating an additional mutation compared to BA.2.86. The study by Cao Yunlong’s team also found that the ability of pre-existing antibodies in the participants’ bodies to neutralize JN.1 decreased by about half.
According to information from the U.S. CDC, common symptoms of JN.1 infection include fever, chills, cough, shortness of breath, difficulty breathing, fatigue, muscle aches, headache, loss of taste or smell, sore throat, runny nose, nausea, vomiting, and diarrhea.
The virology expert mentioned earlier pointed out that the damage caused by COVID-19 infection to the immune system is temporary and can recover over time. Additionally, previous natural infections and vaccine-induced antibodies still provide cross-protection. For those who recover within the normal course of the disease, if they are re-infected with JN.1, the symptoms are generally milder, and there is no need for excessive concern.
However, a second infection is not friendly to vulnerable populations such as the elderly and those with underlying conditions, especially those who have experienced severe infections. Their recovery from physical damage is often slow, and a second infection may have an “accumulative effect” with residual symptoms from the previous infection.
Zhang Zhenhua, director of the Department of Infectious Diseases at the Second Affiliated Hospital of Anhui Medical
University, told “Medicine” magazine that a series of studies show that COVID-19 may not be a simple respiratory disease. It causes damage to the human body in multiple ways and should be treated as a systemic infection.
In mid-December, an article in “The Lancet Infectious Diseases” pointed out that within 18 months after COVID-19 infection, patients face an increased risk of death, rehospitalization, and multiple organ health risks. About half of the deaths occur more than 30 days after infection.
Updated Vaccines Effective:
WHO is continuously monitoring evidence and will update risk assessment reports for JN.1 as needed. It suggests that, for countries entering the winter season, the simultaneous spread of the new coronavirus and other pathogens may exacerbate the burden of respiratory diseases.
On December 14, the U.S. CDC issued a warning to healthcare institutions, stating that hospitalization rates for influenza and respiratory syncytial virus (RSV) had increased by 200% and 60%, respectively, in the previous four weeks. The rate of emergency visits for pediatric pneumonia has been steadily increasing from September to the present.
From U.S. data, the declining willingness to get vaccinated provides conditions for the rapid spread of JN.1. As of December 9, only about 18% of adults in the country had received the latest version of the COVID-19 vaccine.
Based on comprehensive information, WHO proposes that vaccines containing XBB components have cross-reactivity against various variants, including JN.1, and can prevent severe outcomes or death resulting from infection. Currently, China has approved the use of six COVID-19 vaccines containing XBB components. The National Health Commission stated that when the population has broad immunity to the Omicron variant (including vaccination and natural infection), the transmission capacity of the JN.1 variant may be relatively limited.
Jiang Qingwu, a professor at the School of Public Health at Fudan University, emphasized in an interview the need to pay high attention to protecting the elderly and recommending the most effective vaccines for this age group. According to data from Singapore, since the beginning of the year, more than 85% of patients hospitalized due to COVID-19 infection have been in the 60 and above age group.
“The season of respiratory infectious diseases is here, and the medical and public health sectors need to be prepared technically and materially,” Jiang Qingwu said.
“Vaccination with booster shots and obtaining Paxlovid is becoming less common,” said Alex Greninger, assistant director of the Clinical Virology Laboratory at the University of Washington in the United States. Paxlovid is an oral antiviral drug for COVID-19 that, when used within 5 days of infection, can reduce hospitalization rates and decrease the risk of death.
“Not using these tools would be tragic,” emphasized Alex Greninger.
WHO Raises Attention Level for JN.1: Do We Need to Worry About COVID-19 Again?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



