Food-as-Medicine Program Falls Short in Improving Diabetes Control
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Food-as-Medicine Program Falls Short in Improving Diabetes Control
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Food-as-Medicine Program Falls Short in Improving Diabetes Control
Clinical Trial Results Show the U.S. “Food-as-Medicine Program” Doesn’t Improve Hemoglobin A1c Levels in Type 2 Diabetes Patients.
The conclusion that “dietary therapy can’t save diabetes” was surprising to see in the results of a clinical trial because it contradicts the common belief that lifestyle adjustments, such as dietary changes, are effective for diabetes.
Upon closer examination, it becomes clear that this clinical trial pertains to a U.S. program called the “food-as-medicine program,” which is a food security assistance initiative. Given the increasing incidence of chronic diseases related to diet, the program aims to assist individuals who have difficulty accessing safe and healthy food, thereby improving public health and reducing healthcare costs.
Published in “JAMA Internal Medicine,” the paper discusses the small-scale results of the program specifically targeting individuals with type 2 diabetes. Participants in the program received access to healthy ingredients, health guidance, and disease education. Unfortunately, after a follow-up of one year, although participants’ health awareness had increased, there was no significant improvement in glycated hemoglobin (HbA1c) levels.

The participants in this trial were diagnosed with type 2 diabetes and had HbA1c levels of 8% or higher, facing food security issues. The trial utilized a waitlist design, randomly assigning participants to either the treatment or control group. The treatment group could immediately participate in the program, while the control group joined after six months, with a total follow-up period of one year. The program provided healthy ingredients for ten meals per week to the entire household, along with nutritionist consultations, health guidance, and regular diabetes-related checks for participants.
Among the 349 participants included in the analysis at six months, the median age was 55.4 years, with 53.6% being female, and a baseline median HbA1c level of 10.29%.
According to self-reports, the assistance program significantly increased participants’ health consciousness. At the six-month follow-up, the treatment group showed a significant increase in weekly vegetable intake (6.3 vs. 4 times/week), a higher percentage of people not consuming fast food (43.3% vs. 36.3%), and reduced intake of sugary beverages (2.8 vs. 3.4 times/week). However, these data did not show significant statistical differences.
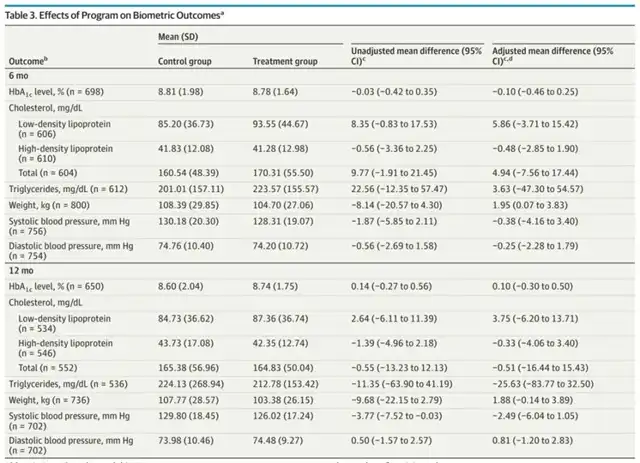
Despite the increased health awareness and substantial material assistance, the treatment group participants did not gain more “health.” At six months, both the treatment and control groups showed significant reductions in HbA1c levels, 1.5% and 1.3%, respectively, with no significant difference after adjusting for influencing factors. The results were consistent at the 12-month follow-up.
Other laboratory test results, including cholesterol, triglycerides, and fasting blood sugar levels, did not show significant changes.
Even though health awareness increased, and tangible assistance was provided, why did it not translate into health benefits?
Researchers suggest that the program only provided participants with ingredients but did not address the difficulties in preparing food afterward. It seems that participants might not know what foods are healthy, or whether cooking at home is better than ordering takeout, considering time, money, and cooking skills.
A scholar commenting on the paper’s official website also noted that the program did not specify the dietary composition. According to previous research evidence, a predominantly plant-based, low-fat diet can effectively improve diabetes issues. If the program only offers “free food” to participants, it can only solve some food security issues and may not address the broader aspects of dietary improvement needed for managing diabetes.
Food-as-Medicine Program Falls Short in Improving Diabetes Control
Reference:
[1]https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2812982
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



