Treatment and Prognosis of Different Pathological Types of Thyroid Cancer
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Treatment and Prognosis of Different Pathological Types of Thyroid Cancer
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Treatment and Prognosis of Different Pathological Types of Thyroid Cancer
Thyroid cancer is the most common malignant tumor of the endocrine system. Over the past two decades, the incidence of thyroid cancer has shown explosive growth in the vast majority of countries and regions worldwide.
There has long been a belief that thyroid cancer is a “lazy cancer.” However, the so-called “lazy cancer” is not a medical term; essentially, it corresponds to low-risk papillary thyroid carcinoma, which progresses relatively slowly and has a good prognosis.
The World Health Organization (WHO) classifies thyroid cancer into papillary carcinoma, follicular carcinoma, medullary carcinoma, and undifferentiated carcinoma. These four types cover over 95% of all thyroid cancers, with papillary and follicular carcinomas collectively referred to as differentiated carcinomas.
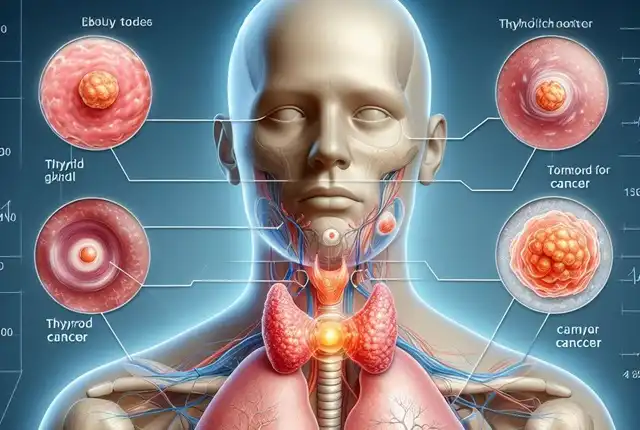
Different pathological types of thyroid cancer imply differences in treatment and prognosis.
1. Papillary Carcinoma
Papillary thyroid carcinoma is the most common differentiated malignant tumor of the thyroid, accounting for approximately 85% of all thyroid cancers. It has the lowest malignancy, with slow tumor growth, often remaining localized within the thyroid for several years, but with a high rate of local lymph node metastasis. Papillary thyroid carcinoma has the best prognosis among thyroid cancers. It usually does not present obvious clinical symptoms and is typically detected through thyroid palpation and ultrasound. When the tumor is large, it can cause compression symptoms such as difficulty breathing and swallowing. Invasion of local nerves can lead to symptoms such as hoarseness and difficulty swallowing. Metastasis to cervical lymph nodes can also cause noticeable neck masses.
Treatment and Prognosis: Since papillary thyroid carcinoma is insensitive to chemotherapy and radiotherapy, surgical removal is the most important and effective initial treatment. Thorough surgical excision is the fundamental treatment for papillary thyroid carcinoma. Depending on the extent of thyroid tumor lesions, either unilateral thyroid lobectomy with isthmusectomy or total thyroidectomy is chosen, with central lymph node dissection or neck lymph node dissection based on the presence of cervical lymph node metastasis. With the continuous development of surgical techniques, the emergence of minimally invasive and endoscopic surgeries has brought new options for patients with cosmetic needs. Patients with papillary carcinoma who undergo surgical treatment have a high survival rate, and postoperative adjuvant iodine-131 therapy can be used for late-stage patients with lymph node metastasis.
The prognosis of papillary carcinoma is excellent, with a 10-year survival rate exceeding 90%, reaching over 98% in younger individuals. Factors affecting prognosis include age and sex (low-risk group: males <40 years, females <50 years; high-risk group: males ≥40 years, females ≥50 years), tumor size and number (>5cm, poor prognosis; ≤1.5cm, excellent prognosis; multifocal, poor prognosis), tumor capsule and margin (no capsule and diffuse growth, poor prognosis), thyroid capsule (extrathyroidal invasion, poor prognosis), metastasis (distant metastasis, poor prognosis), presence of vascular and neural invasion (vascular or neural invasion, poor prognosis), and nuclear atypia (significant atypia, poor prognosis).
2. Follicular Carcinoma
Follicular thyroid carcinoma is the second most common type of thyroid cancer. Follicular and papillary carcinomas have similar origins, differentiation statuses, clinical prognoses, and treatment modalities, hence often collectively referred to as differentiated thyroid carcinoma. Follicular carcinoma accounts for approximately 5.9% of all thyroid cancers. Overall, it has a lower malignancy, but approximately 10% to 30% of patients may experience distant metastasis, leading to a poor prognosis. Follicular carcinoma less frequently metastasizes to lymph nodes than papillary carcinoma and may undergo early hematogenous dissemination, spreading to the lungs, liver, bones, and central nervous system through blood vessels. Metastasis to bones may cause bone pain and pathological fractures, while metastasis to the brain may result in dizziness, headaches, and other symptoms of central nervous system involvement. Therefore, the clinical presentations of follicular carcinoma with metastases may vary.
Treatment and Prognosis: The treatment of follicular carcinoma is similar to that of papillary carcinoma, with surgical treatment being the common approach. The prognosis is worse than that of papillary carcinoma but better than that of medullary and undifferentiated carcinomas. The standardized treatment of differentiated thyroid carcinoma primarily involves surgery, followed by determining the subsequent treatment plan based on tumor staging and risk of recurrence. The main components include:
- Surgical excision of the primary lesion and possible excision of metastatic lesions.
- Some patients may require radioactive iodine-131 therapy to destroy residual thyroid tissue after surgery and occult or inoperable metastatic lesions.
- Most patients need to take thyroid hormone tablets for life to supplement thyroid hormone, suppress tumor recurrence, and growth.
3. Medullary Carcinoma
Medullary thyroid carcinoma originates from parafollicular cells (C cells) of the thyroid and has a low incidence, accounting for only 2% to 3% of all thyroid cancers. Medullary carcinoma can be classified as sporadic or familial. Sporadic cases account for about 70% of all medullary carcinomas and are more common in individuals aged 50 to 60 years, while familial medullary carcinoma is an autosomal dominant inherited disease, accounting for approximately 30% of all medullary carcinomas and occurring at a relatively younger age.
Medullary thyroid carcinoma lacks papillary or follicular structures and is characterized by nests or cystic arrangements of undifferentiated cells; amyloid deposits may be present in the tumor, with potential invasion of cervical lymph nodes and hematogenous metastasis. Regardless of sporadic or familial occurrence, the prognosis of medullary carcinoma is worse than that of differentiated thyroid carcinoma. Most patients present with painless thyroid nodules at the initial diagnosis, with some patients also experiencing cervical lymphadenopathy. Special symptoms include tetany and paresthesia if blood calcium levels decrease. Calcitonin and carcinoembryonic antigen (CEA) are derived from parafollicular cells of the thyroid and can secrete “calcitonin,” a hormone that lowers serum calcium levels. Therefore, significantly elevated levels of serum calcitonin (CT) may serve as a “signal” for medullary carcinoma. However, due to the regulatory effects of other mechanisms in the body (such as parathyroid hormone and the kidneys), blood calcium levels generally do not decrease significantly. Additionally, the level of carcinoembryonic antigen (CEA), a commonly used tumor marker, may also increase.
Treatment and Prognosis: Surgery is the primary treatment, with radiotherapy and chemotherapy showing limited efficacy. Surgical excision is currently the only effective treatment for medullary carcinoma. The surgical approach usually involves total thyroidectomy with prophylactic central lymph node dissection. Postoperatively, radioactive iodine-131 therapy is generally not necessary unless the lesion contains components of differentiated thyroid carcinoma (papillary or follicular carcinoma). Regular follow-up examinations are required postoperatively to monitor serum levels of carcinoembryonic antigen and calcitonin, which help monitor tumor recurrence. Over 50% to 90% of patients can survive for more than 10 years.
4. Undifferentiated Carcinoma
Undifferentiated thyroid carcinoma is the type of thyroid cancer with the worst prognosis, with a median survival time of only 5 to 10 months. It consists of highly invasive malignant tumors composed of undifferentiated thyroid follicular cells. Typical symptoms include rapidly enlarging, hard, fixed neck masses with extensive invasion of surrounding tissues. Approximately 30% to 40% of patients have distant metastases, such as to the lungs, bones, and brain. Overall, the treatment of undifferentiated carcinoma is challenging. Many patients are diagnosed with distant metastases, and effective treatment options are limited. If resection is possible, surgery remains the preferred treatment option. However, extensive surgery is not helpful in prolonging survival if the tumor has already invaded important organs such as the trachea and esophagus or if distant metastases exist.
Treatment and Prognosis of Different Pathological Types of Thyroid Cancer
(source:internetlfmi2AEzLR2MeaH65DpbwA, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



