2022 USCAP Thyroid Disease Pathology Hotspot Contents
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
2022 USCAP Thyroid Disease Pathology Hotspot Contents
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
2022 USCAP Thyroid Disease Pathology Hotspot Contents.
In PTC with an STI component, encapsulation/invasion status was a determinant of lymph node metastasis and DFS, but not STI percentage.
Non-invasive encapsulated tumors with an STI component are indolent with very low risk of lymph node metastasis and recurrence.
The overall prognosis of PTC with STI is good, with a 10-year disease-free survival rate of 89%.
Head and neck and endocrine pathology thyroid histopathology-related content was presented at this meeting, including 2 presentations:
- 2022 5th edition WHO thyroid tumor pathological classification update, DICER1-related thyroid tumors ;
- 2 platforms (Platform Session) : Two thyroid cancer clinical studies (thyroid NUT cancer, solid papillary thyroid cancer); 13 poster sessions (Poster Session).
This article summarizes the report and platform presentation.
On the afternoon of March 21, the two platforms of endocrine pathology held two thyroid cancer clinical studies.
1. Professor Steven Gilday of Brigham and Women’s Hospital, Harvard Medical School lectured on “thyroid NUTM1-rearranged cancer as a distinct and less aggressive subtype of NUT cancer”.
Background:
NUT carcinoma is a rare subtype of squamous cell carcinoma, defined by NUTM1 gene fusions (the most common fusion partners are BRD4, BRD3, and NSD3, found in approximately 80%, 15%, and 5% of cases, respectively).
It usually occurs in young patients with head and neck or midline thoracic structures and has a poor prognosis, with a median survival of 6.5 months and a 2-year overall survival rate of 19-22%. Cases of thyroid NUT cancer are rarely reported.
Methods:
We studied 9 cases of thyroid NUT cancer diagnosed between 1999 and 2021, and analyzed their clinicopathological features, immunohistochemical features, NUTM1 fusion partners and their prognosis.
Thyroid NUTM1 Rearranged Cancer, from Professor Steven Gilday’s courseware
Results:
The median age at diagnosis was 35 years (17-72 years), including 6 female patients and 3 male patients. The mean tumor size was 4.4 cm (2.5-6.0 cm).
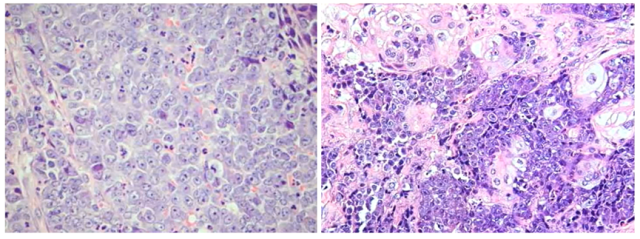
Of these, 4 (44%) were diagnosed as NUT carcinoma at biopsy or excision, 3 were diagnosed as poorly differentiated thyroid carcinoma (PDTC), and 2 were diagnosed as anaplastic thyroid carcinoma (ATC). Squamous differentiation was present in 57% of cases (4/7; 2 without biopsy).
Of the cases with immunohistochemical results, all cases (4/4) were NUT positive, 57% (4/7) TTF1 positive, 40% (2/5) PAX8 positive, 75% (3/4) P63 or P40 positive.
Four PD-L1 staining showed a composite positive score of 1% or higher (range 5-100). The NUTM1 fusion partner was NSD3 in 6 (67%), BRD4 in 2 (22%), and unknown in 1 (11%).
7 cases underwent total or partial thyroidectomy (obvious extrathyroidal infiltration was seen in all cases), and 2 cases only underwent biopsy.
At diagnosis, 7 patients had lymph node metastases and 1 patient had distant metastases (3 patients were indeterminate).
At last follow-up, only 2 patients died of disease (3.5 and 31 months after diagnosis), 3 patients survived with disease, and 3 survived disease-free (median last follow-up time of surviving patients was 36.2 months).
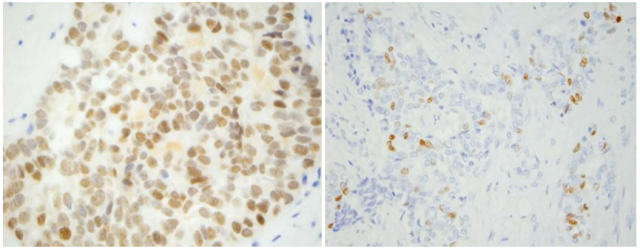
Median overall survival was not reached in this cohort. For patients with adequate follow-up, the 2-year survival rate was 83%.
Thyroid NUTM1 rearranged cancer positively expresses NUT and expresses P63 to varying degrees, from the courseware of Professor Steven Gilday
Conclusion:
Thyroid NUT carcinoma may overlap with PDTC and ATC in histomorphological and immunohistochemical features, with high NSD3-NUTM1 fusion rate and longer survival than typical NUT carcinoma.
Overall survival rate of thyroid NUTM1 rearranged cancer, from the courseware of Professor Steven Gilday
2. Professor Bin Xu of Memorial Sloan Kettering Cancer Center gave a lecture on “Redefining Papillary Thyroid Carcinoma of Solid Type (PTC-SV): A Multicenter Retrospective Study”.
Background:
PTC-SV is considered an aggressive subtype of PTC. But in the definition of PTC-SV, the solid/trabecular/island structure (STI) varies from >50% to nearly 100%.
In addition, ≥30% STI structures can rule out the diagnosis of non-invasive thyroid follicular tumor with papillary nuclei features (NIFTP).
This multicenter retrospective study aimed to establish thresholds for STI components in PTC-SV and to identify prognostic factors for PTC with STI components.
Methods:
A retrospective study of 120 cases of PTC with different proportions of STI components was performed.
The prognosis was determined based on the risk of lymph node metastasis and recurrence-free survival (RFS).
For multifocal tumors, only the largest tumors with STI structures were included.
RESULTS:
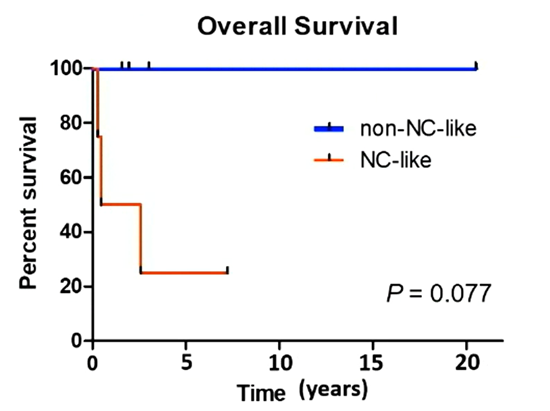
The risk of lymph node metastasis was significantly associated with encapsulation/infiltration (P < 0.001), but not with the STI ratio (P = 0.781).
N1 lymph node metastases were found in 1-3% of encapsulated PTCs and 43-59% of invasive PTCs, regardless of STI percentage.
Other parameters associated with lymph node metastasis were papillary and follicular structure percentage, vascular invasion, margin status, extrathyroidal invasion (ETE), and AJCC pT stage.
Distant metastasis occurred in 6 patients, and local recurrence occurred in 2 patients. The 10-year DFS in the entire cohort was 89 %, with encapsulated lesions in 98 % and invasive tumors in 75 %.
STI percentage was not associated with DFS (P = 0.239). Other important prognostic factors included vascular invasion, histological and macroscopic extrathyroidal invasion, AJCC pT and pN stages, and tumor size.
Fifty patients with noninvasive encapsulated lesions had a 2%-100% STI component. Thirty-five patients did not meet the diagnostic criteria for NIFTP due to the presence of nipples (n=3), ≥30% STI (n=29), or 3-4 mitotic images/10 high-power fields (n=3).
In 1 patient with 2.7 cm diameter tumor consisting of 80% STI component and 4 classic micropapillary carcinomas, psammoma was found in the central lymph node. No patient relapsed.
In 76 patients, RAS mutation and BRAF V600E mutation detection showed that encapsulated lesions were rich in RAS mutations (54%), while invasive lesions lacked RAS mutations (4%).
BRAF V600E mutations are rare, found only in 11% of all cases, 8% of encapsulated lesions, and 17% of invasive lesions.

Invasive and non-invasive thyroid tumors with STI structures, from Prof. Bin Xu’s courseware
CONCLUSIONS: In PTC with an STI component, encapsulation/invasion status was a determinant of lymph node metastasis and DFS, but not STI percentage.
Non-invasive encapsulated tumors with an STI component are indolent with very low risk of lymph node metastasis and recurrence.
The overall prognosis of PTC with STI is good, with a 10-year disease-free survival rate of 89%. Therefore, it is recommended to reconsider whether to classify SV-PTC as an aggressive PTC subtype in order to save patients from unnecessary invasive treatments.
Further studies are needed to reassess the 30% STI threshold in the NIFTP exclusion criteria.
2022 USCAP Thyroid Disease Pathology Hotspot Contents
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



