Cell: Obesity suppresses immune cells and accelerates tumor growth
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
Cell: Harvard Medical School confirmed that obesity suppresses immune cells and accelerates tumor growth
Cell: Obesity suppresses immune cells and accelerates tumor growth. In today’s society, with economic development and improvement of living standards, obesity has become a major public health problem worldwide. According to statistics from the World Health Organization (WHO), nearly 2 billion people are overweight or obese in the world. From 1975 to 2016, the global obesity rate has nearly tripled. Every year, overweight or obesity causes 2.8 million deaths.
In fact, obesity is not only a feature, but also a disease. Obese people not only have inconvenience in life and decreased exercise capacity, but are also more susceptible to metabolic diseases and cardiovascular and cerebrovascular diseases. In addition, many studies have shown that obesity is associated with more than ten types of cancer The increased risk of disease is related to the decreased prognosis and survival rate.
Over the years, scientists have determined that metabolic changes and chronic inflammation caused by obesity will drive tumor growth, but the interaction between obesity and cancer is still elusive.
On December 9, 2020, researchers from Harvard Medical School and other units published in the top international academic journal Cell titled: Obesity Shapes Metabolism in the Tumor Microenvironment to Suppress Anti-Tumor Immunity (Obesity affects the metabolism in the tumor microenvironment, Thereby suppressing anti-tumor immunity) research papers.
The study showed that obesity can reduce the number of important immune cells CD8+ T cells and anti-tumor activity in tumors. This is because cancer cells will reprogram their metabolism in response to the increase in fat, so as to better consume energy-rich fat molecules, deprive T cells of energy supply, and accelerate tumor growth.
More importantly, the research team discovered a protein called PHD3. PHD3 protein can inhibit excessive fat metabolism. Overexpression of PHD3 protein can effectively reverse the suppression of tumor immune cells by high-fat diet, which is expected to become a new target for cancer treatment.
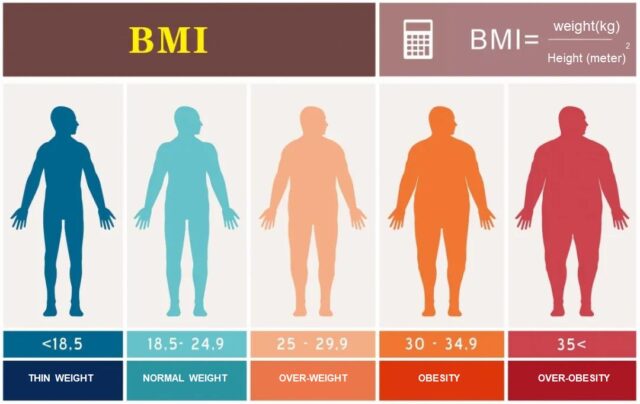
Definition of obesity
The BMI index, or body mass index, is a commonly used international standard to measure the degree of body weight and health. BMI = weight (Kg) divided by height squared (m2). A BMI index greater than 25 is considered overweight, and greater than 30 is considered obese.
Obesity leads to insufficient energy supply of T cells in tumors
In order to reveal the effect of obesity on cancer, the research team conducted research on mouse models with different cancer types. The test results showed that high-fat diet can cause obesity in mice, and the obesity induced by high-fat diet damages the tumor microenvironment. CD8+ T cell cells accelerate tumor growth.
Further experiments showed that diet-related differences in tumor growth depend in particular on the activity of CD8+ T cells. If CD8+ T cell cells in mice are eliminated through experiments, the diet will not affect the growth rate of tumors.
Surprisingly, a high-fat diet reduces the presence of CD8+ T cells in the tumor microenvironment, but does not reduce the CD8+ T cells in other parts of the body. The remaining CD8+ T cells in the tumor are less robust, divide more slowly, and have signs of decreased activity. However, when these cells are separated and grown under laboratory conditions, they have normal activity again, which indicates that some substances in the tumor weaken the function of CD8+ T cells.
Specifically, under a high-fat diet, cancer cells can reprogram their metabolism to increase fat uptake and utilization, while CD8+ T cells cannot. Eventually, certain fatty acids in the tumor microenvironment are depleted, making CD8+ T cells unable to Obtain this necessary energy source.
The first author of the study, Alison E. Ringel, said that the abnormal consumption of fatty acids is one of the most surprising findings in this study, which shows that obesity can change the way in which different cells in tumors use energy sources. In this direction, Both shocking and exciting.
Discover potential therapeutic targets
Next, the research team used several different methods, including single-cell gene expression analysis, large-scale protein analysis, and high-resolution imaging. The research team determined the diet-related metabolic pathways in tumor cells and immune cells in the tumor microenvironment. Variety.
Among these metabolic changes, PHD3 is of particular interest. In normal cells, PHD3 inhibits excessive fatty acid metabolism. The research team found that cancer cells in an obese environment have significantly reduced PHD3 expression.
The research team overexpressed PHD3 in cancer cells. As a result, the ability of tumor cells in obese mice to metabolize fat decreased, the free fatty acids in the tumor microenvironment increased, and more importantly, the number of CD8+ T cells in the tumor recovered.
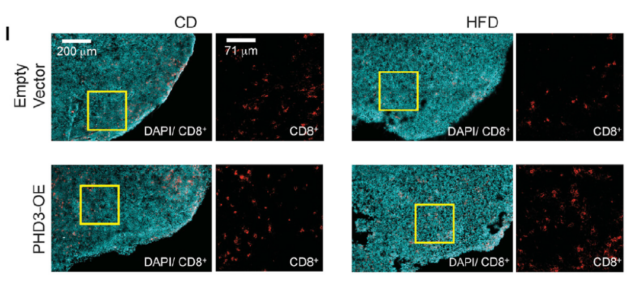
Cyan is tumor tissue, red is CD8+ T cell
In general, this study found and confirmed that obesity can reduce the number of important immune cells CD8+ T cells and anti-tumor activity in tumors. This is because cancer cells will reprogram their metabolism in response to the increase in fat, so as to better consume energy-rich fat molecules, deprive T cells of energy supply, and accelerate tumor growth.
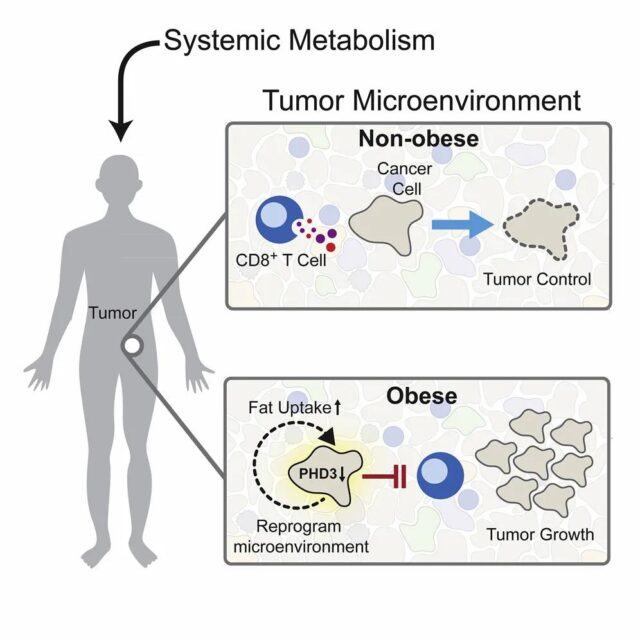
More importantly, the research team discovered a protein called PHD3. PHD3 protein can inhibit excessive fat metabolism. Overexpression of PHD3 protein can effectively reverse the suppression of tumor immune cells by high-fat diet, which is expected to become a new target for cancer treatment.
In recent years, the development of cancer immunotherapy is greatly affecting the lives of cancer patients. However, cancer immunotherapy does not benefit everyone. This study shows that there is a metabolic tug-of-war between T cells and tumor cells, and who is dominant changes with obesity. This can help scientists start thinking about cancer immunotherapy and combination therapies.
These results also lay the foundation for a better understanding of how obesity affects cancer and the impact of patient metabolism on treatment outcomes.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



