What is the result if we let virus and cancer cells fight each other?
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
What is the result if we let virus and cancer cells fight each other?
What is the result if we let virus and cancer cells fight each other? Sub-Journal of “Nature”: Two “killer” viruses and cancer cells that threaten human health, who will die when the two meet?
Oncolytic virus is a kind of tumor-killing virus with replication ability. Because it can stimulate the body to produce anti-cancer immune response without harming normal healthy tissues, it has gradually become a new star in the field of anti-tumor therapy.
In the early 20th century, “The Lancet” magazine reported that a woman with chronic leukemia showed signs of a decrease in the number of diseased white blood cells and improvement of her condition after an influenza virus infection, which attracted the attention of the scientific community. In 1991, an article in “Science” magazine officially opened the prelude to the oncolytic virus entering the anti-cancer circle. For the first time, human beings genetically modified the oncolytic virus and used it for malignant glioma.
However, the birth of this “anti-tumor sword” was not smooth. In 2005, the world’s first anti-cancer oncolytic virus “H101 (Ankerui)” was launched in China, but the cancer treatment effect was not satisfactory, and then gradually “Retreat from the rivers and lakes”, it was not until the FDA approved the birth of the first oncolytic virus therapy to treat melanoma in the United States in 2015 that the oncolytic virus’s anti-cancer road was officially opened.
However, oncolytic virus therapy also has its shortcomings. When the therapy is used independently, the tumor cannot be completely regressed. The fundamental reason is that each cancer patient has a different sensitivity and response to oncolytic virus. Therefore, in order to allow Cancer patients benefit from this therapy, and effective identification of the genetic characteristics of the host susceptible to virus infection has become the top priority of current research.
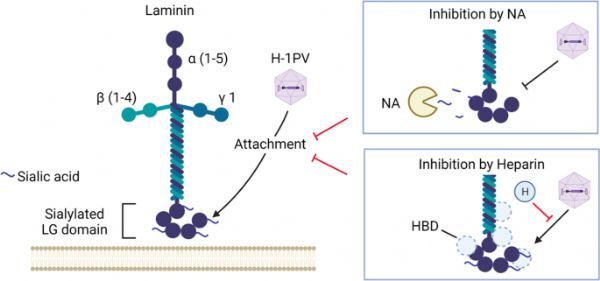
Recently, researchers from the German Cancer Research Center and the oncolytic virus immunotherapy laboratory jointly published an article entitled Oncolytic H-1 parvovirus binds to sialic acid on laminins for cell attachment and entry in the journal Nature Communications. The study found the “laminin”, the gateway for viruses to enter cancer cells, and clarified how H-1 parvovirus (H-1PV) attaches and sneaks into cancer cells, causing tumors to lyse and die.
In order to use oncolytic viruses more effectively and find biomarkers that help identify H-1PV susceptibility, the research team analyzed the protein genes located on the surface of cancer cells to characterize their role in the process of docking with the virus.
Laminin γ1 (LAMC1), a regulator that plays a key role in mediating cell attachment and penetration, is locked. In essence, when the virus interacts with a specific part of the cancer cell, the layer on the surface of the cancer cell Adhesin is like a “door”, it can help the virus track, attach and destroy cancer cells. Studies have found that when LAMC1 is inactivated in environments such as glioma, cervical cancer, pancreatic cancer, colorectal cancer and lung cancer, the virus’s aggressiveness to cancer cells will be weakened.
In further research, researchers evaluated the clinical significance of this new discovery. The researchers pointed out that laminin is differentially expressed in different tumor microenvironments. For example, compared with healthy tissues, it is overexpressed in pancreatic cancer and glioblastoma (GBM).
In addition, in brain tumors, its expression will increase with the increase of tumor grade, and the level of laminin in tumors of patients with advanced GBM is higher. Not only that, 110 biopsy analysis reports of primary and recurrent GBM showed that compared with the primary tumor, the level of laminin in recurrent GBM was significantly higher.
However, it is gratifying that although the increased expression of laminin is associated with the prognosis and poor survival of a variety of tumor patients, it can make tumors more susceptible to infection and destruction, that is to say, the high expression of laminin Cancer patients are more likely to respond to oncolytic virus therapy.
Therefore, in the future, we can use laminin as a biomarker to classify cancer patients based on its expression level in order to predict the sensitivity and responsiveness of different types of cancer to H-1PV-based anti-cancer therapies.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



