Overview of the treatment of midbrain glioma
- Gut Bacteria Enzymes Offer Hope for ABO Universal Blood Transfusions
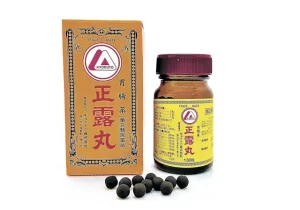
- Well-Known Japanese Medicine Exposed for 30 Years of Data Falsification
- Oregon Reverses Course: From Decriminalization to Recriminalization of Drug Possession
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
Overview of the treatment of midbrain glioma
Overview of the feasibility of treatment of midbrain glioma, how to diagnose, how to treat, and how to prognosis?
1. What is midbrain glioma?
The midbrain is part of the brainstem, located above the pons, the top of the brainstem, and just below the cerebellum. The midbrain is one of the most important components of the central nervous system (CNS) and is the connection point between the central and peripheral nervous systems. All neurotransmission through the body and the entire peripheral nervous system (PNS) to the central nervous system must pass through the midbrain [1].
The midbrain is related to many functions of the nervous system, and its functions extend to many different parts of the central and peripheral nervous system, from motor to sensory and cognitive abilities.

Midbrain gliomas occur in the midbrain and are usually not surgically removed because they are located deep in the brain. Tumors can be benign or malignant; they can be primary or metastatic. Common tumors in the midbrain include hemangioblastoma, ganglioglioma and ependymoma. Midbrain tumors mostly occur in children and are divided into childhood benign gliomas and juvenile malignant gliomas. If it is malignant, the prognosis is often poor. Midbrain tumors account for 1-2% of brain tumors in children and are not common in adults. The incidence of midbrain tumors is basically the same in both sexes. The incidence of glioma in patients with brainstem tumors is 10.3% [1], and tectal tumors are more common than tectorial tumors.
Symptoms of midbrain tumors include visual impairment, ataxia, nausea and hemiplegia. Some patients may be asymptomatic. Gliomas that occur in the midbrain are usually of low grade (Grade I) and are mostly benign. Low-grade benign astrocytomas can often be surgically removed, and the prognosis is good. High-grade midbrain glioma (HGG), such as diffuse midline glioma (an aggressive and incurable brain tumor in children), is characterized by resistance to antitumor drugs due to the intact blood-brain barrier It is difficult to treat [2]. When surgery is not feasible, the treatment is usually radiotherapy or chemotherapy.
Mesencephalic glioma is considered to be “may be the tumor that causes the least death in the human body.” The death of patients is mostly due to obstructive hydrocephalus caused by the tumor, rather than the tumor itself. Symptoms and signs of hydrocephalus may include: nausea, vomiting, irritability, headache, blurred vision, lethargy, and epilepsy.

How to diagnose?
MRI (MRI) is the preferred method for diagnosing midbrain tumors. The introduction of MRI imaging has improved the accuracy of diagnosis. MRI imaging can identify important imaging features and multi-planar positioning of tumors. It allows accurate assessment of tumor growth patterns and accurate preoperative diagnosis in most cases. Similarly, postoperative MRI shows the effect of resection, distinguishing residual and recurring tumors, and showing tumor changes [2]. Functional imaging such as proton MRI spectroscopy is an effective tool to distinguish low-grade and high-grade gliomas.
What are the treatment options for midbrain glioma?
The treatment strategy is based on clinical manifestations.
1. Neurosurgical treatment
If possible, the preferred treatment for midbrain glioma should be surgery. The purpose of surgery is to obtain tissue to determine the type of tumor, and to remove as many tumors as possible without causing more damage to the patient. The brainstem, thalamus, and spinal cord are sensitive parts of the central nervous system, and surgery on these parts can cause severe functional loss. Low-grade brainstem glioma has a clear boundary in the midbrain, and neurosurgical resection should be considered. If the risk of biopsy is too high, radiotherapy alone can be used instead of biopsy [3]. If the patient has hydrocephalus, surgery such as ventricular shunt will be required to redirect the flow of cerebrospinal fluid.
For most pediatric patients, the lesions are usually clinically and radiologically stable. Only proper treatment of obstructive hydrocephalus is required. Cerebrospinal fluid (CSF) shunt surgery is generally recommended.

For adult patients, conservative treatment, observation and symptom control are recommended. Surgical treatment should be reserved for patients with obstructive hydrocephalus. Unless there is imaging or clinical evidence that the tumor has evolved, specific treatment should be selected. The manifestations of focal, non-enhancing, and non-exogenous lesions are similar to benign tectal tumors in children. These focal mesencephalic gliomas have clear edges, slow growth, and are generally inert in nature. In most cases, Removal is appropriate.
2. Adjuvant treatment
Patients usually require further treatment after surgery. This may include radiotherapy, chemotherapy or clinical trials. In most cases, radiation therapy is given after surgery. Chemotherapy is sometimes given at the same time as or after radiotherapy. However, there is currently no standard chemotherapy regimen. Each regimen should be specific to each patient. A review of the condition by a neurosurgeon or expert is very important to determine the best treatment plan. Clinical trials, new chemotherapy, targeted therapy, and immunological drug therapy are all within the possible treatment options.
Prognosis
The volume and location of midbrain tumors are highly related to the prognosis. Surgery removes as much tumors as possible, and postoperative radiotherapy is beneficial to patients.
Focal gliomas in the midbrain tectum and tectum have a better prognosis than diffuse gliomas that extend to the brainstem. Patients with focal midbrain glioma require treatment for persistent hydrocephalus.
Although most patients have not achieved total resection, the tumor seems to evolve slowly or disappear after surgery. Therefore, good clinical results and long-term patient survival seem to be available.
(source:internet, reference only)
Disclaimer of medicaltrend.org