NOAC: insufficient evidence for left ventricular thrombosis
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
NOAC: insufficient evidence for left ventricular thrombosis
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- What is the difference between Atorvastatin and Rosuvastatin?
- How long can the patient live after heart stent surgery?
NOAC: insufficient evidence for left ventricular thrombosis.
New oral anticoagulants (NOAC) are widely used in deep vein thrombosis and pulmonary embolism, but there is still insufficient evidence in left ventricular thrombosis after acute myocardial infarction.
Left ventricular thrombosis is a complication of acute myocardial infarction (AMI) and, if left untreated, is associated with a significant risk of thromboembolism.
The incidence of left ventricular thrombosis in AMI, especially in patients with acute anterior myocardial infarction, can reach 2.7% to 12.3%, and even in patients with acute ST-segment elevation myocardial infarction (STEMI) (11.5% to 43%).
The current guidelines (ESC, ACCF/AHA, ACCP) all recommend the use of vitamin K antagonists (VKA) for anticoagulation therapy for 3 to 6 months.
New oral anticoagulants (NOAC) are widely used in deep vein thrombosis and pulmonary embolism, but there is still insufficient evidence in left ventricular thrombosis after acute myocardial infarction.
Research Introduction
There are currently studies comparing the safety and effectiveness of NOACs and VKA in the treatment of left ventricular thrombosis in patients with AMI.
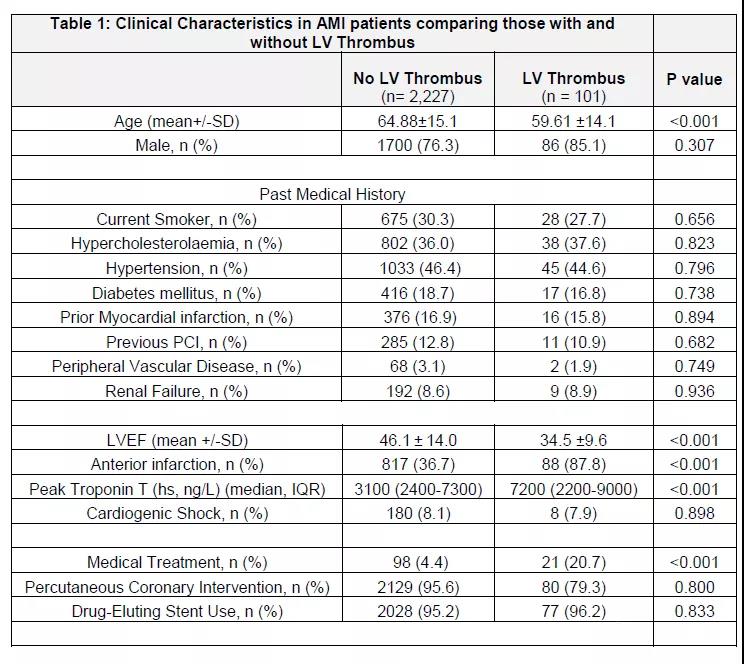
The study included 2328 consecutive patients who underwent coronary angiography +/- percutaneous coronary intervention (PCI) diagnosed as AMI at the British Heart Center from May 2015 to December 2018. The primary endpoint is the rate of left ventricular thrombolysis; the secondary endpoint is the rate of bleeding.
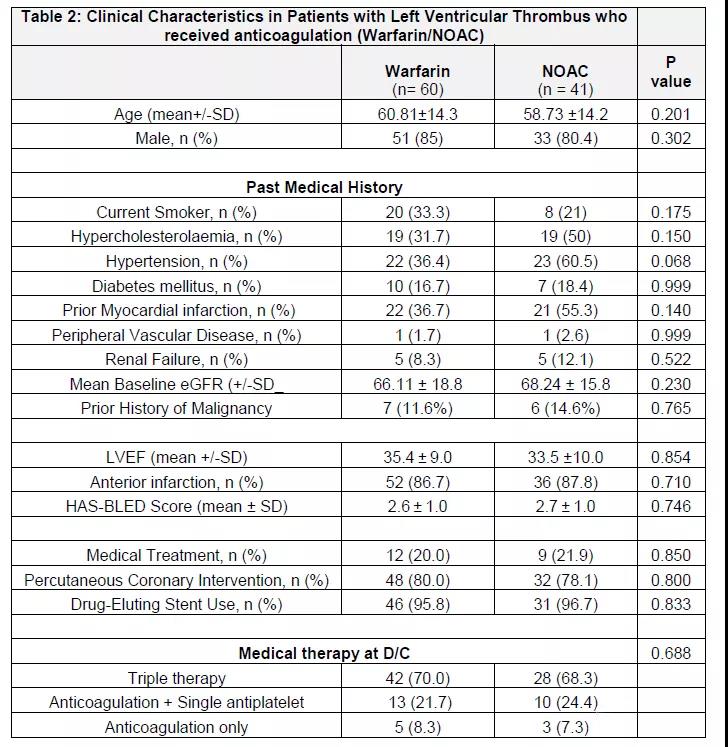
The results of the study suggested that 101 patients (4.3%) were diagnosed with left ventricular thrombosis. Sixty patients (59.4%) started VKA treatment, and 41 patients (40.6%) received NOAC treatment (including rivaroxaban: 58.5%, apixaban: 36.5%, and idoxaban: 5.0%).
The two groups were matched to baseline, including age, previous history of heart disease (previous myocardial infarction, PCI, coronary artery bypass graft) cardiovascular risk factors (hypertension, diabetes, hypercholesterolemia).
In addition to dual antiplatelet therapy, patients diagnosed with left ventricular thrombosis after AMI are treated with VKA or NOAC on the second to sixth day of hospitalization.
The anticoagulation treatment plan is determined by the attending physician.
The dose of NOAC is used according to the patient’s condition (such as renal function, etc.). Patients taking warfarin keep the international normalized ratio (INR) range at 2.0-3.0.
During the follow-up period (median 2.2 years), the overall rate of left ventricular thrombosis resolution was 86.1%.
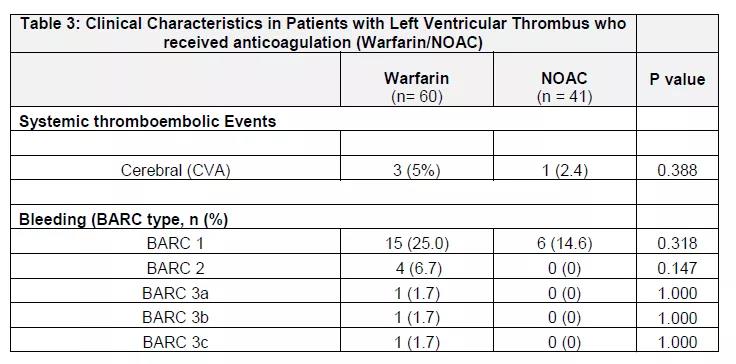
At 1 year, the rate of left ventricular thrombolysis in the NOAC group was higher than that in the warfarin group (82% vs 64.4%, P=0.0018, 1 year).
This difference still exists after adjusting the baseline variables after surgery (OR: 1.8, 95%CI: 1.2~2.9). Major bleeding events were significantly lower in the NOAC group than in the VKA group (0% vs 6.7%, P=0.03).
There was no difference in the incidence of systemic thromboembolism between the two groups (5% vs 2.4%, P=0.388).
This study suggests that in the treatment of left ventricular thrombosis after AMI, NOAC patients may have better therapeutic effects and safety than VKA patients.
However, the sample size of this study is still small, and the treatment plan is non-random, so there may still be great confounding factors, and dabigatran treatment is not used in the NOAC plan, so this conclusion may not apply to all NOACs.
NOAC: insufficient evidence for left ventricular thrombosis.
(source:chinanet, reference only)
Disclaimer of medicaltrend.org



