Pfizer COVID-19 vaccine still effective for coronavirus variants?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Pfizer COVID-19 vaccine still effective for coronavirus variants?
Pfizer COVID-19 vaccine still effective for coronavirus variants? Is the COVID-19 vaccine VS virus mutation still useful? Here are two good news…
Recently, in the wave of the outbreak of the COVID-19 epidemic in the South Asian subcontinent, good news about vaccines against the COVID-19 variants is constantly being reported. “Nature” reported the performance of Pfizer vaccine against B.1.351 (South Africa variant) in Qatar on May 6, local time. At the same time, The Wall Street Journal reported that China’s Kexing vaccine was in Brazilian Serrana’s performance against P.1 (Brazilian mutant).
Nature’s report on Pfizer vaccine against mutant strains, screenshots are from Nature’s official website
Regrettably, B.1.617 (Indian variant), which has received much attention, has not yet been reported on the statistical data of vaccine and its resistance. Whether the vaccine can outperform the mutation seems to be caught in controversy…
Good news for the UK and South Africa variants
In the process of promoting vaccination, Qatar has experienced the peak of B.1.1.7 (the British variant) in March, and the aggressive expansion of B.1.351 that began in mid-March. As of March 31, a total of 385,853 people in Qatar have received at least one shot of the vaccine, and 265,410 people have completed two shots of immunization.
The effectiveness of Pfizer vaccine is estimated from a sample survey of the above population. The specific data are as follows:
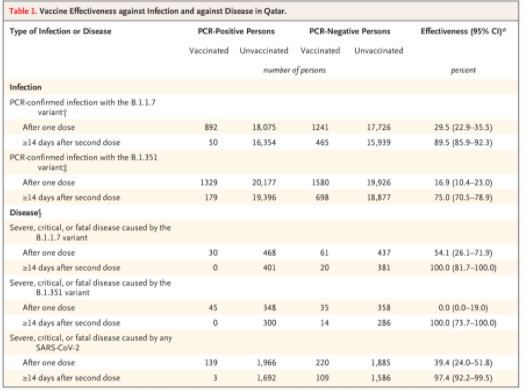
This batch of data was released to NEJM on May 5, local time.
The figure shows that in the B.1.1.7 group, the sample size of the two injections is 515, among which 50 people still have B.1.1.7 infection two weeks after completing the two injections. After the analysis of the Pfizer vaccine completed the immunization , The effective rate of B.1.1.7 is 89.5%, and if only one injection is injected, it is only 29.5%. This shows that one shot cannot achieve herd immunity against B.1.1.7.
In group B.1.351, 179 people were infected two weeks after the completion of two injections of the vaccine, and 698 people were not infected. Data analysis showed that the vaccine effective rate was 75.0%. Similarly, if only one shot is vaccinated, the effective rate is 16.9%, and herd immunity cannot be achieved.
In other words, according to this data, as long as enough people complete the two injections in time, Pfizer vaccine can form an effective herd immune barrier against the British and South African mutants.
Another good news is that 14 days after complete Pfizer vaccination, the number of severe and fatal cases for the above two variants dropped to zero. Even the data covering other local new coronavirus variants show that after complete vaccination with Pfizer, the protection rate against severe and fatal conditions reached 97.4%.
As of March 31, 6,689 people in Qatar were infected with the COVID-19 after receiving a single shot of Pfizer, 1616 people were infected after two shots, and only 7 people died after being vaccinated with COVID-19, of which 5 people received only 1 shot. The next 2 deceased completed 2 shots of vaccination.
At the same time, Serrana, Brazil, also heard good news about vaccines. Serrana is located in the southeast of Brazil, in the north of São Paulo State, with a population of about 45,600. The famous P.1 was among the new coronaviruses that raged in the city. In the past three months, most of the people in the city who can get the vaccine have basically completed the Kexing vaccine immunization.

Aerial view of Serrana
Excluding minors under the age of 18, pregnant women, breastfeeding women, and patients with major diseases, there are about 27,700 adults who can be vaccinated in the city, of which 27,160 have completed two immunizations.
Official Serrana statistics show that the local COVID-19 infection rate has dropped by 75% from the peak in March. At present, there are no cases of death after infection of COVID-19 among those who have completed the immunization. In addition, according to local officials, the local hospital was still overcrowded before the second immunization was completed. After the second immunization, the number of hospital admissions was greatly reduced. In April this year, Serrana died of 6 people due to the COVID-19 infection, 5 of them received only one shot of the vaccine, and the remaining 1 died two days after completing the second shot.
Since the personnel responsible for the vaccine research have not yet released detailed data, the specific protection rates have not yet been officially announced, and the relevant personnel expressed optimistic expectations. Previous phase III clinical studies have shown that Kexing vaccine has a 50% protection efficiency against symptomatic infections of the new coronavirus, and a 100% protection against death. The person in charge of this study believes that the medical staff selected for the Phase III clinical trial of Kexing is different from sampling samples of other vaccines. Because medical staff are more likely to be exposed to the virus, the data result may be lower than that of Kexing vaccine. The results in the general population, Serrana’s real-world data will provide further support for the effectiveness of the vaccine.
Vaccines VS India variants, can vaccines still effective?
The record of the above two vaccines against the British variants, the South African variants and the Brazilian variants seems to give people a sigh of relief for the effectiveness of the vaccine. So, what about the Indian mutant?
There is no conclusion yet, including whether India will continue or have produced new mutant strains is temporarily unknown.
The known information is that there are three variants of B.1.617, all of which have now arrived in the UK. Public Health England (PHE) currently considers B.1.617.2 among them to be the most noteworthy, because the increase in the number of people who have detected this variant among infected persons in the United Kingdom is increasing, and some researchers believe that it is similar to the British variant. Communication ability.
PHE recently announced information that a cluster infection occurred in a nursing home in the UK. 15 elderly people who had completed the vaccination were confirmed to be infected with B.1.617.2. Fortunately, the infected are gradually recovering and no deaths have occurred.
Compared with these elderly people, Rajendra Kapila, an American expert on infectious diseases, is not so lucky. On April 28 this year, he studied infections for a lifetime and was the founder of the New Jersey Infectious Diseases Society. He died of infection with COVID-19 in India. Before going to India, he had completed the COVID-19 vaccine immunization in the United States.

abc News report on the matter
His wife Deepti Saxena-Kapila is a microbiology expert working in the United States. She told the media that she has been researching COVID-19 on the front line in the past year and has protected her family from infection. She never expected to go to India for 2 weeks. The husband fell ill and soon developed to death.
There is no public information about Kapila’s specific condition. Some sources believe that Kapila is 81 years old and suffering from type 2 diabetes, with cardiovascular complications, which may be the cause of his severe illness and death after infection. Current data from Pfizer Vaccine in the United States shows that among the 105 million people who have completed two doses of immunization, only 70 reported cases of death after being infected with the nCOVID-19. Most of the patients who died were elderly and had underlying diseases.
In addition, it is worth noting that in the recent G7 foreign ministers meeting, two of the Indian delegation tested positive for the COVID-19. Although the conditions of the two people and the virus strains were not disclosed in detail, the situation is quite thought-provoking. After all, Indian officials of this level should have completed the vaccine immunization, and shouldn’t they carry out nucleic acid testing before leaving the country… …
With the spread of the epidemic in India to neighboring countries, reports of B.1.617 infection after completion of vaccine immunization gradually appeared in neighboring countries, and the battle between vaccine and B.1.617 must continue to wait and see.
Has the vaccine ever mutated? Just look at whether humans will drag each other back?
Although several major mutant strains in the world continue to occupy the news section of the epidemic in turn, it is not just them that the vaccine has to fight against, but the continuous mutation trend of the new coronavirus itself.
Last year, some researchers sent out preprints with confidence, believing that recovered patients have neutralizing antibodies and will not be infected again. At the beginning of this year, the second wave of the outbreak in Manaus, Brazil completely denied this possibility, making these preprints only preprints forever.
Local multi-angle statistics show that in the first wave of the epidemic in Manaus last year, the collective infection rate exceeded 70%, and a study of local blood donors showed that 76% carried neutralizing antibodies. The analysis of the Manaus epidemic paper published by The Lancet pointed out that even taking into account factors such as the decline in antibodies in recovered patients, when the second wave of the epidemic broke out, 52.5% of the locals should carry neutralizing antibodies produced after natural infections. , If these antibodies work, a second wave of infection frenzy is unlikely to occur, which means that it is very likely that some people with neutralizing antibodies will have re-infection…
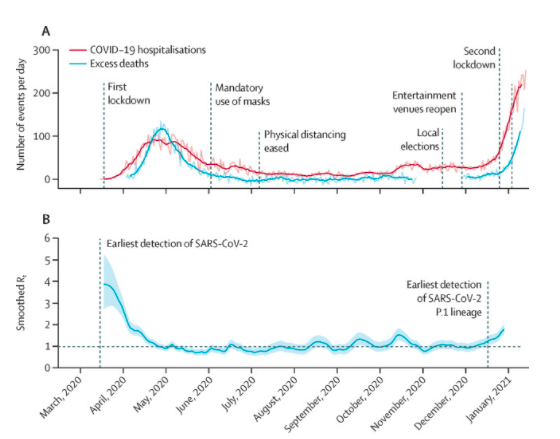
The Brazilian Manaus infection data published by The Lancet shows that there was a more severe outbreak at the beginning of this year than in May last year, and the increase in hospital admissions and deaths far exceeded the peak last year.
Since P.1 was discovered in Manaus slightly earlier than the second wave of outbreak, some analysis believes that the situation in Manaus means that neutralizing antibodies formed by past infections may not be able to fight against new mutations.
This is also a question that vaccines have to consider-can they fight against mutant strains? If not, can the speed of research and development and immunity catch up with the speed of mutation?
The Science journal published a study on the mutation of COVID-19 in mid-April. This article brought some good news and some bad news.
The study published by Picture Science mainly takes the infection situation in the UK as a sample
The bad news: Studies have found that even without the pressure of treatment and vaccine selection, the new coronavirus can undergo adaptive mutations with sufficient frequency in the host.
The good news: Most mutations did not get the chance to spread, and many mutant strains have silently disappeared before they got the chance to spread on a large scale.
Good news X2: In the early stage of infection, when the viral load is high, it is more difficult to increase the transmission power or the mutation of the immune escape ability.
Bad news X2: Although the emergence of mutant strains with enhanced transmission power or immune escape ability is irregular, once the opportunity for transmission is obtained, it will spread quickly and on a large scale.
In short, the meaning of this paper is that the new coronavirus mutates extremely fast and undergoes high-frequency adaptive mutations in the host, but many mutant strains have not obtained the opportunity to spread. Those fierce mutant strains with immune escape ability Once it gets the opportunity to spread, it will soon “occupy the market.” The researchers also called for in their conclusions that all parts of the world should share virus data and transmission data as much as possible, in order to track and fight virus mutations faster and better through research.
However, this is also a problem. Not to mention some conspicuous areas where the epidemic is clearly anxious but is almost a black hole of data. Recently, Nature even wrote an article to emphasize and analyze the problem of researchers in many areas actively refusing to share virus data. Yes, not without , It is not unconditional to share, but “Yes, but refuse to share”…

On May 5, local time, Nature issued a report reporting that researchers in some areas voluntarily refused to share new coronavirus data
The Nature report pointed out that many researchers who refuse to share data are in underdeveloped areas. They believe that their results have been shared by researchers in developed countries and regions, and they have not benefited from it, even in past epidemics. , The vaccine developed by handing over the samples of the country cannot be returned to the majority of the people in the country who are trapped in poverty. Therefore, no matter how much researchers and related institutions in developed countries and regions call for the public benefit of sharing data, some regions always refuse to share. However, due to poor public health management and epidemic prevention capabilities, these regions are likely to be difficult to deal with. Variant strain.
This ironic situation is really sighing. It is so difficult to fight the virus alone, and humans have to drag each other back in mutual harm…
At present, there are two aspects to the situation of vaccines and virus mutations. The first is to see who covers the population quickly. The more people who are infected, the more the virus can mutate. Therefore, in virus-endemic areas, the speed of vaccine coverage is the key-traveling against the current-vaccine coverage is slower, and virus coverage is faster and mutates faster; the second is to develop new vaccines and develop supplements After the completion of the development, there is a new round of vaccination and mutation speed racing against the current.
If the vaccine coverage speed is not enough to form an immune barrier, then the battle between the vaccine and the COVID-19 may be like Sisyphus pushing a stone, pushing it up and rolling down, endlessly repeating the cycle, and be careful not to cause ADE in the process.
A recent article in the New York Times of the United States pointed out that there is little hope of achieving herd immunity through vaccine immunization in the United States. Experts have observed that when the basic data is far from meeting the requirements for herd immunity, the number of daily vaccine injections in the United States Is declining. Therefore, the herd immunity barrier that was originally scheduled to be achieved this summer is now basically hopeless-and due to the emergence of variants that enhance transmission, the original herd immunity threshold has to be raised, making the goal more difficult to reach.
NYT’s report on vaccine immunization and epidemics in the United States
The article predicts that the COVID-19 virus will exist in the United States for a long time, and there will still be hospitalizations and deaths due to it-but the number is much smaller than before there was no vaccine. The article also pointed out that vaccine immunization should continue. Even if herd immunity cannot be achieved, more people will be injected with the vaccine to help reduce the severe illness and mortality caused by the COVID-19 infection-thereby reducing the risk of medical runs, and ultimately within one or two generations. , To control COVID-19 as a long-standing infectious disease like the flu.
Finally, with regard to the formulation of epidemic prevention strategies, one important factor has to be mentioned-economy. Just as countries have placed their economic impact and strategies such as non-aggregation, isolation, and lockdown on the balance, the high economic income of the COVID-19 vaccine is a fact, and several vaccine research and development manufacturers that have published financial reports have greatly increased their vaccine revenue. This year’s revenue forecast. Under such circumstances, will the formulation of vaccine strategies be affected by economic factors like isolation or lockdown?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



