Bayer Vitrakvi: Targeted drugs for various cancers with long-lasting effect
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Targeted anti-cancer drugs! Bayer Vitrakvi has a long-lasting effect in the treatment of TRK fusion cancers of all age groups & various tumors.
Bayer Vitrakvi: Targeted drugs for various cancers with long-lasting effect. Bayer recently released 4 new data from analysis, confirming the long-term clinical characteristics of Vitrakvi (larotrectinib), a precision oncology drug, including: Vitrakvi’s long-term clinical characteristics in all age groups (range: 0.1-84 years) and multiple tumor types TRK fusion cancer patients have rapid, highly durable remission and good tolerability.

These analyses include the latest long-term efficacy and safety data in non-primary central nervous system (CNS) solid tumors, primary CNS tumors, and lung cancer carrying NTRK gene fusion.
In addition, an intra-patient retrospective analysis showed that most patients with TRK fusion cancer received Vitrakvi treatment to obtain meaningful clinical benefits.
Based on the largest data set and the longest follow-up time for TRK inhibitors, with a median follow-up time of 22.3 months, Vitrakvi showed sustained high remission rates and more than surpasses in NTRK gene fusion cancer patients of all ages and different tumor types. 4 years of remission durability.
Vitrakvi is a pioneering, potent, oral, and selective tropomyosin receptor kinase (TRK) inhibitor, designed to directly target TRK (including TRKB, TRKB, and TRKC) and shut down the signal that leads to TRK fusion tumor growth path. When an NTRK gene is fused with another unrelated gene to produce an altered TRK protein, TRK fusion cancer will occur.
The altered protein, or TRK fusion protein, becomes constitutively active or overexpressed, triggering the activation of the intercellular signaling cascade. These TRK fusion proteins act as drivers of oncogenes and promote the spread and growth of tumors. TRK fusion cancers are generally rare, can affect children and adults, and occur at different frequencies in different tumor types. TRK fusion-driven tumors can occur in various parts of the body, and conventional treatment options (such as surgery, chemotherapy, radiotherapy, etc.) usually cannot achieve satisfactory treatment results.
Vitrakvi is the first “unrestricted cancer type, broad-spectrum” oral targeted anticancer drug that has nothing to do with tumor type. It is specifically used to treat various tumors carrying NTRK gene fusion, regardless of where the tumor originated in the body. In children and adult patients with TRK fusion tumors, Vitrakvi has a strong therapeutic effect, including for primary central nervous system (CNS) tumors and brain metastases, providing high remission rates and long-lasting remissions, regardless of the patient’s age and tumor histology .
At the end of November 2018, Vitrakvi received the world’s first batch in the United States, becoming the first oral TRK inhibitor approved in history. At present, Vitrakvi has been approved in many countries around the world for the treatment of children and adult patients with advanced or metastatic solid tumors with NTRK gene fusion in the tumor. Just recently, in accordance with the latest announcement from the Center for Drug Evaluation (CDC) of the National Medical Products Administration (NMPA), Bayer has submitted Vitrakvi’s marketing application in China.
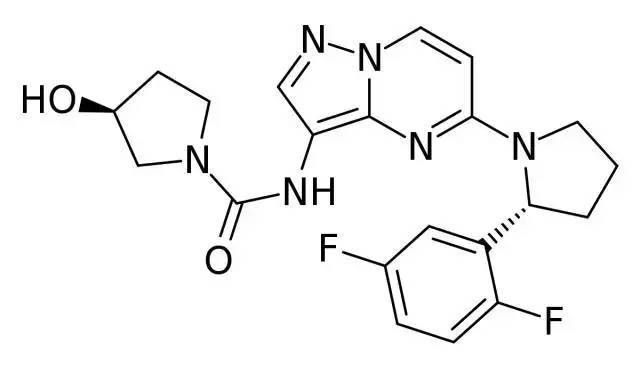
Larotrectinib molecular structure
1. Larotrectinib adult and child comprehensive data set (Abstract 3108)
An extended data set for long-term follow-up (deadline: July 20, 2020) evaluated 206 adult and pediatric patients with TRK fusion carcinoma covering 21 different tumor types, showing the investigator’s assessed overall response rate (ORR) It was 75% (95%CI: 68-81), and the complete remission rate (CR) was 22% (n=45).
For patients with evaluable brain metastases (n=15), the ORR was 73% (95%CI: 45-92). Among all evaluable patients, the median follow-up was 22.3 months, and the median duration of response (DOR) was 49.3 months (95%CI: 27.3-not estimable [NE]).
At a median follow-up of 20.3 months, the median progression-free survival (PFS) was 35.4 months (95%CI: 23.4-55.7). At a median follow-up of 22.3 months, the median overall survival (OS) had not yet been reached, and the 36-month OS rate was 77% (95%CI: 69-84).
The safety profile was consistent with the overall safety profile previously reported, and no new safety signals were found. Most of the reported treatment-related adverse events (TRAE) were mainly grade 1 or 2, and 18% of patients reported grade 3 or 4 TRAE. Larotrectinib was discontinued in 2% of patients due to TRAE, and no treatment-related deaths were reported.
The data of the integrated dataset comes from 3 larotrectinib clinical trials (NCT02122913, NCT02576431, NCT02637687) carried out in adult and pediatric patients with TRK fusion cancer. The analysis does not include the primary central nervous system (CNS) patient subgroup.
2. Larotrectinib in the treatment of lung cancer with or without CNS metastasis (Abstract 9109)
The latest analysis data of adult lung cancer patients with TRK fusion carcinoma who have previously received multiple therapies (median previous therapies: 3) (deadline: July 20, 2020) show that larotrectinib has high activity, rapid and durable remission , Prolonged survival period, good long-term safety.
Among the 15 evaluable patients, according to the investigator’s assessment, the confirmed ORR was 73% (95% CI: 45-92), and among the evaluable patients with baseline CNS metastasis (n=8) the ORR was 63% ( 95%CI: 25-91). Among all evaluable patients (n=15), the 12-month sustained response rate (DOR) and progression-free survival rate (PFS) were 81% and 65%, respectively.
The median follow-up was 16.2 months, and the median overall survival (OS) was 40.7 months (95%CI: 17.2-NE). There were 16 patients with TRAE, and 2 of them had Grade 3 events. No patient stopped taking larotrectinib due to TRAE. These data are evaluated by the investigator and come from patients in 2 clinical trials (NCT02576431, NCT02122913).
3. Larotrectinib in the treatment of patients with primary CNS tumors (Abstract 2002)
In another report (deadline: July 20, 2020), 33 patients with primary CNS tumors in children and adults carrying NTRK gene fusions from 2 clinical trials (NCT02637687, NCT02576431) were evaluated with larotrectinib.
Most (82%) patients with measurable diseases experienced tumor shrinkage, with an ORR of 30% (95% CI: 16-49), and a 24-week disease control rate of 73% (95% CI: 54-87). The median follow-up was 16.5 months, the median PFS was 18.3 months (95%CI: 6.7-NE), and the median OS did not reach (95%CI: 16.9-NE). The 12-month OS rate was 85% (95%CI: 71-99). Grade 3 or 4 TRAE occurred in 3 cases. No patient stopped taking larotrectinib due to TRAE.
4. Comparison of intra-patients in clinical trials of larotrectinib in the treatment of TRK fusion cancer (Abstract 3114)
Other larotrectinib data to be presented at the conference include an updated and expanded retrospective growth regulation index (GMI) analysis, which is limited to patients in the larotrectinib trial who have received at least one therapy.
GMI is a retrospective comparison of the patient’s self. The patient is used as a control by comparing the PFS of the current treatment with the time to progression or treatment failure (TTP) of the most recent previous treatment. GMI ratio ≥ 1.33 has been used as a threshold for meaningful clinical activity.
In the long-term follow-up analysis of 122 patients (as of July 2020), almost three-quarters of patients had GMI ≥ 1.33, including 6 of the 9 patients with GMI ≤ 1.33 in the previous analysis.
In the extended data set of 140 patients, 74% of patients had GMI ≥ 1.33. The data comes from 3 larotrectinib clinical trials (NCT02122913, NCT02576431, NCT02637687).
(source:internet, reference only)
Disclaimer of medicaltrend.org



