Will COVID-19 Omicron become a “flu” after its virulence declines?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Will COVID-19 Omicron become a “flu” after its virulence declines?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Will COVID-19 Omicron become a “flu” after its virulence declines?
Nature confirms that Omicron is “reduced in virulence”, what impact will it have on epidemic prevention?
On May 16, Nature published a blockbuster study, which for the first time provided comprehensive evidence for the weakening of the virulence of the Omicron variant in an in vivo model.
The study found that compared with the early circulating new coronavirus strains, the Omicron BA.1 and BA.2 variant strains (hereinafter referred to as BA.1 and BA.2) have limited ability to infect mouse or hamster lungs, and the severity of the disease significantly reduced. At the same time, several current therapeutic monoclonal antibodies and antiviral compounds can effectively inhibit Omicron.
In fact, real-world infection data has provided evidence for the decline of Omicron’s virulence before relevant experimental studies have been released one after another. The most direct is the weakening of “pulmonary phagocytosis”, and there is no longer a high correlation between “COVID-19 infection” and “initiation of pneumonia”.
Therefore, more and more people are comparing “Omicron” with “flu virus”, will it be another “flu”?
Virus titers in the respiratory tract
More than a hundred times lower than the original strain
The research was jointly completed by dozens of scientists from many universities and research institutions in Japan and the United States. One of the corresponding authors is Yoshihiro Kawaoka, a foreign academician of the American Academy of Sciences and a virologist.
In the experiment, BA.2 mutants isolated from Japan were selected and infected with mice and hamsters respectively. Compared with mice, hamsters are closer to the metabolism of the human body.
The study showed that neither mice nor hamsters infected with BA.1 and BA.2 observed significant weight loss. Two measures of lung function, the airway narrowing index (PenH) and the ratio of peak expiratory time (Rpef) , also did not change significantly.
Histopathological analysis of mouse lungs revealed that BA.1 and BA.2 were significantly less infectious in the lungs than infecting beta mutants and only induced a limited pulmonary inflammatory response.
Further experiments were performed in humanized k18-hACE2 transgenic mice , a more susceptible mouse , and found that at similar infection doses, BA.1 and BA.2 were infected:
- Infectious virus titers in the respiratory tract were 270-830-fold lower than infecting the original strain, while viral RNA levels in the lungs and nose showed similar declines.
- Levels of most proinflammatory cytokines and chemokines were significantly lower in the lungs than in the original strain.
After lung imaging examination of infected hamsters, it was found that compared with the early new coronavirus, the lungs of hamsters infected with the Omicron variant showed only very mild abnormalities, which was equivalent to “slight pneumonia”, while half of the hamsters did not. develops a lung infection.
A more sensitive hamster model was then used to evaluate the original strain at a dose of “10% body weight loss and 100% death after 5 days”:
- The survival rate of infection with BA.1 and BA.2 reached 75% and 100%, respectively, and the virus titer in the lung after BA.1 infection was 10,000-fold lower than that of the original strain.
- The researchers believe that this shows that the pathogenicity of BA.1 and BA.2 has been significantly weakened, and the replication ability of BA.2 in the lower respiratory tract has been significantly reduced.
Current treatments still work
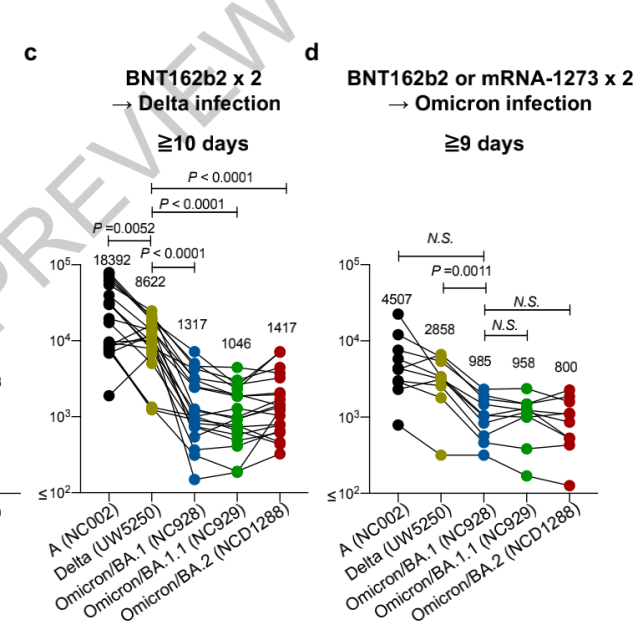
The investigators also assessed the neutralizing activity (FRNT) of live BA.2 virus against vaccinated, or combined breakthrough sera from individuals with breakthrough infection .
It was found that the neutralizing activity against the Omicron family after three doses of mRNA vaccine was significantly lower than that against the delta strain and the original strain, and the geometric mean titer FRNT50 differed by 2.8 to 6.6 times.
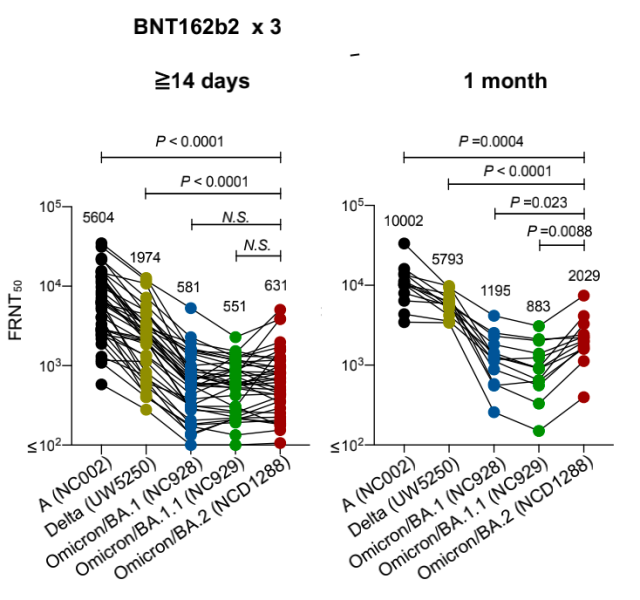
Even after being vaccinated with two mRNA vaccines and then infected with the Omicron variant, the neutralizing activity of the plasma to the Omicron family after 9 days was lower than that of the delta variant.
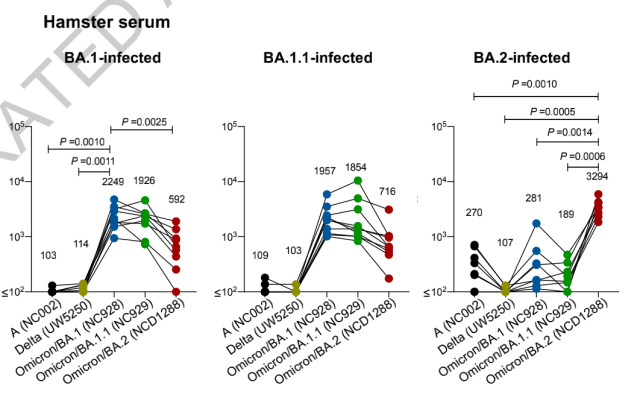
To further evaluate the antigenic properties of BA.2, the researchers found through hamster experiments that infection with BA.2 could not stimulate broad-spectrum plasma neutralizing activity, and the geometric mean titer of BA.1 was only 1/12 of that of BA.2, indicating that BA. The antigenicity of .2 is not only different from other mutants, but also has great differences even within the Omicron family.
The good news is that several therapeutic monoclonal antibodies and antiviral compounds are still effective against Omicron. In hamster treatment experiments, REGN10987/REGN10933, COV2-2196/COV2-2130 and S309 restricted BA.2 replication in the lung.
In terms of antiviral compounds, Molnupiravir, Nirmatrelvir, and S-217622 all significantly reduced viral titers in the lung, and S-217622 also exhibited viral inhibitory efficacy in the nose.
Omicron’s virulence declines, will it become a “flu”?
Optimists believe that the arrival of the Omicron variant provides “an opportunity” for humans to return to normal life.
The virus will not disappear out of thin air, and people will have to defend against the virus threat in the future through extensive vaccination, specific drugs, and autoimmunity acquired after infection. During this period, the reduction in viral virulence helps reduce the health cost to humans.
But the road doesn’t look smooth right now.
“It’s more of a numbers game,” Professor Leif Erik Sander, an infectious disease expert at the Charlotte Medical School in Germany, told Science.com.
Even though the number of cases causing serious illness is relatively small, new infections could still make health problems worse. The system is overwhelmed.
Another point that is different from the flu virus is that Omicron is reducing human expectations for building a “vaccine barrier”, and the trend is getting stronger. BA.2.12.1, BA.4, BA.5, the former taking the US by storm, and the latter two have become the main popular variants in South Africa.
In the early days of the Omicron variant, according to its reduced virulence, there is a view in the academic community that infection with Omicron is equivalent to a “natural booster needle”. But at present, at least in the prevention of breakthrough infection, the effect of this “natural booster needle” is very limited.
On April 30, 2022, domestic universities and medical research institutions, including Peking University and Beijing Ditan Hospital, published a paper on the preprint platform bioRxiv, pointing out that BA.2.12.1 showed stronger binding to human ACE2 receptors The ability of the three new variants to evade humoral immunity was further improved on the basis of BA.2 in the face of the plasma of vaccine recipients.
This means that as major vaccine manufacturers try to keep up with changing trends and develop a new generation of vaccines, the evolution of the new coronavirus may have left these efforts behind.
“The evolution of Omicron may continue to adjust until all the improvement methods are exhausted.” Professor Benjamin tenOever, professor of microbiology at New York University, also said in an interview with the media.
“The core problem is that the coronavirus has become better at reinfecting people.” The New York Times published an article on May 16 that early people believed that the new coronavirus may, like the flu , break out once a year, most likely in the fall. Early vaccination can reduce its spread.
The situation is changing, and experts are quoted in the article. Vaccines are increasingly limited and the immune response to infection is so weak that infection with one virus does not leave much protection against other variants.
“When ‘reinfection’ becomes the norm, outbreaks are not just an annual, and their morbidity and mortality rates suggest more than a ‘minor trouble’.”
Melanie Ott, a virologist at the Gladstone Institutes in the United States, told the health website “STAT” that what is happening now may be a preview of the future.
“One variant starts to spread, causing an increase in cases. When parts of the population re-establish more effective immune protection, the virus evolves, again being replaced by another variant that outperforms it,” she said.
What should we do?
On May 2, 2022, experts from the FDA’s Center for Biologics Evaluation and Research published an article in the Journal of the American Medical Association, saying that the COVID-19 vaccination will become the norm every year.
Since real-world data still shows that vaccines are especially protective for high-risk groups, an evaluation and decision on “who should be revaccinated first” and “what route/brand of COVID-19 vaccine” should be made before the fall, the article said.
Despite the reduced potency, experts believe the Covid-19 vaccine should be updated more quickly than the flu vaccine.
Even if it is not an exact match with the new variant strain, immunity can be expanded and some protection can be provided.
Linfa Wang, a researcher at the National University of Singapore School of Medicine, believes that a broad range of monoclonal antibody drugs against different strains may be the best way to deal with it, especially for those who have low immunity and vaccines cannot be effective.
“The downside is the cost, which is about $1,000 per patient for a dose of monoclonal antibody,” he said. “Whether anyone can find a way to bring that down to $50 or $100.”
Going further, single responses are waning, even strict non-pharmaceutical interventions (NPIs) – which have had great success in China over the past two years, but as the virus’s basic reproduction number (R0) climbs, the cost of Also rising.
On May 10, researchers from the School of Public Health of Fudan University published a modeling article in Nature Medicine on the prevalence of Omicron variants in China, proposing that vaccination should be ensured, the availability of antiviral therapy should be increased, and the NPI should be maintained.” Three-pronged approach.”
“None of the above three interventions alone can reduce deaths to influenza levels or avoid ICU runs,” the paper said. “The key to a combined intervention is to increase vaccination rates in the elderly population and to make antiviral therapy more widely available.”
The article puts forward corresponding indicators. When the vaccination rate of the elderly reaches 97%, 50% or more of symptomatic infected persons can receive antiviral treatment, the peak ICU occupancy rate will not exceed the actual carrying capacity, and the total number of deaths will be reduced to the same level as the season. Sexual flu is equivalent.
On the other hand, scientific research is still very important, it can allow humans to keep up with the evolution of the new coronavirus as much as possible, so as to formulate countermeasures in advance.
“STAT” said that there are many factors that trigger the slowdown of the epidemic, including climate, and scientists are focusing on correlating the evolution of the virus and the persistence of human protection with the latest epidemic trends.
On March 14, 2022, the journal Nature Reviews Microbiology commented that so far we know very little about the environment and process by which different variant strains produce different antigenicity, which makes it difficult to predict the timing, antigenicity and properties of future variants. Call for further research.
The article cautions that viral evolution will maximize transmissibility, which may sometimes be associated with higher virulence, such as high viral loads that promote transmission but also increase disease severity.
Cross-species transmission of the virus is another major threat. Compared with repeated infection and mutation in the human population, the virus evolves in animals and then passes back to humans, which may produce new and more “strong” mutant strains.
Earlier this year, a study in the Journal of Biosafety and Biosecurity by a team of experts from the Chinese Center for Disease Control and the Institute of Public Health and Health of Nankai University suggested that Omicron did not evolve from Delta, but may have been Originated in mice, evolved and evolved naturally in the mouse host and then passed back to humans.
Virology expert Chang Rongshan told the “medical community” that the new coronavirus has been found in about 10 species within two years, which may indicate that the frequency of its cross-species is thousands of times that of similar viruses.
We need to strengthen the COVID-19 virus. Related research on virus cross-species transmission. “
references:
[1] Antigenic evolution will lead to new SARS-CoV-2 variants with unpredictable severity, https://www.nature.com/articles/s41579-022-00722-z
[2] COVID-19 Vaccination—Becoming Part of the New Normal, https://jamanetwork.com/journals/jama/fullarticle/2792030?c
[3] BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection, https://www.biorxiv.org/content/10.1101/2022.04.30.489997v1.full
[4] How Often Can You Be Infected With the Coronavirus?, https://www.nytimes.com/2022/05/16/health/covid-reinfection.html
[5] What the current spike in Covid-19 cases could say about the coronavirus’ future, https://www.statnews.com/2022/05/12/what-the-current-spike-in-covid-19- cases-could-say-about-the-coronaviruss-future/
[6]Characterization and antiviral susceptibility of SARS-CoV-2 Omicron/BA.2, https://www.nature.com/articles/s41586-022-04856-1
Will COVID-19 Omicron become a “flu” after its virulence declines?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



