NEJM: Paid sick leave and breast cancer screening
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
NEJM: Paid sick leave and breast cancer screening
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
NEJM: Paid sick leave and breast cancer screening
Cancer screening is effective in improving early cancer detection and prolonging survival. But while the Affordable Care Act eliminated most cost-sharing for cancer screenings, fewer than 70 percent of U.S. adults receive recommended screenings for the two most common cancers: breast and colorectal.
Barriers such as job stress, time constraints, and lost wages are often cited as major factors in the underutilization of preventive care services such as cancer screening, leading researchers to hypothesize that offering paid sick leave to cover cancer screening would improve compliance with cancer screening guidelines. compliance.
The United States is one of two developed countries without a federal mandate guaranteeing workers access to paid sick leave.
The Healthy Families Act of 2004, the first attempt at federal paid sick leave legislation, has since been introduced several times but has yet to become law.
As a result, nearly 30 percent of the nation’s workforce lacks paid sick leave, and low-income workers, women, and underserved racial and ethnic groups have lower paid sick leave coverage.
In the absence of a federal policy, 17 states, including Washington, D.C., four counties and 18 cities have mandated paid sick leave for eligible workers.
As a result, nearly 20 million workers could receive paid sick leave by the end of 2022.
However, the fact that 18 states pre-emptively passed laws prohibiting municipalities from enforcing paid sick leave underscores the controversy surrounding current paid sick leave policies.
Although lack of paid sick leave may impede access to preventive care, the available evidence is insufficient to draw meaningful conclusions about its association with cancer screening.
The few studies analyzing this association generally reported a positive association.
However, these studies typically compared workers with paid sick leave to workers without paid sick leave and thus may have been confounded by selection bias .
For example, workers who are particularly health-conscious are more likely to follow screening guidelines and are more likely to work in jobs that offer paid sick leave.
In this case, the association between paid sick leave and cancer screening would be overstated because it includes both a causal effect of paid sick leave on screening rates and a greater willingness to be screened among health-conscious individuals.
On March 2, 2023, New England Journal of Medicine of the Massachusetts Medical Association, published online A study by the Young Institute for Policy Studies and the University of California, San Francisco School of Medicine overcomes the selection bias problem with a quasi-experimental research design after a policy rationalizes changes in paid sick leave coverage and mandates employers to authorize employees to receive preventive medical services during paid absences .
The research was funded by the National Cancer Institute.
Using administrative health insurance claims data from approximately 2 million private sector employees from 2012 to 2019, the study examined 12-month and 24-month colorectal cancer screening for workers living in metropolitan statistical areas affected by and without paid sick leave policies .
The association between paid sick leave policies and breast and colorectal cancer screening was compared with changes in mammography and mammography screening rates.
As a result, 61 U.S. metropolitan statistical areas (16 percent) were affected by paid sick leave policies during the study period. Before the policy was passed, screening rates were similar across metropolitan statistical areas.
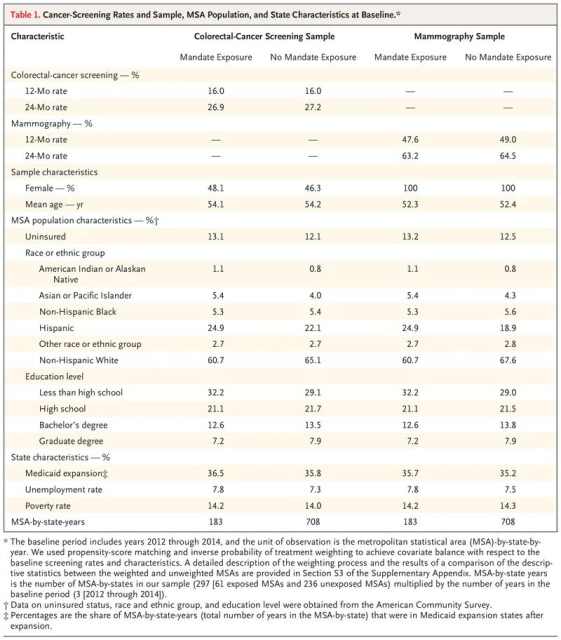
After adjusting for other influencing factors, workers living in metropolitan statistical areas affected versus not affected by the paid sick leave policy:
- The 12-month colorectal cancer screening rate was 1.31 percentage points higher (95% confidence interval: 0.28-2.34)
- The 24-month colorectal cancer screening rate was 1.56 percentage points higher (95% confidence interval: 0.33-2.79)
- The 12-month mammography screening rate was 1.22 percentage points higher (95% confidence interval: -0.20 to 2.64)
- The 24-month mammography screening rate was 2.07 percentage points higher (95% confidence interval: 0.15-3.99)
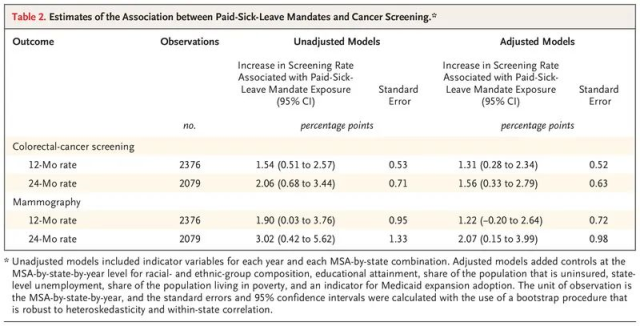
Thus, the results of this study suggest that among U.S. private sector workers, cancer screening rates are significantly higher among workers residing in metropolitan statistical areas with and without paid sick leave policies. Lack of paid sick leave is one of the barriers to cancer screening.
N Engl J Med. 2023 Mar 2;388(9):824-832. IF: 176,079
Cancer Screening after the Adoption of Paid-Sick-Leave Mandates.
Callison K, Pesko MF, Phillips S, Sosa JA.
School of Public Health and Tropical Medicine, Murphy Institute of Political Economy, Tulane University, New Orleans; Andrew Young School of Policy Studies, Georgia State University, Atlanta; School of Medicine, University of California at San Francisco, San Francisco.
BACKGROUND: By the end of 2022, nearly 20 million workers in the United States have gained paid-sick-leave coverage from mandates that require employers to provide benefits to qualified workers, including paid time off for the use of preventive services. Although the lack of paid-sick-leave coverage may hinder access to preventive care, current evidence is insufficient to draw meaningful conclusions about its relationship to cancer screening.
METHODS: We examined the association between paid-sick-leave mandates and screening for breast and colorectal cancers by comparing changes in 12- and 24-month rates of colorectal-cancer screening and mammography between workers residing in metropolitan statistical areas (MSAs) that have been affected by paid-sick-leave mandates (exposed MSAs) and workers residing in unexposed MSAs. The comparisons were conducted with the use of administrative medical-claims data for approximately 2 million private-sector employees from 2012 through 2019.
RESULTS: Paid-sick-leave mandates were present in 61 MSAs in our sample. Screening rates were similar in the exposed and unexposed MSAs before mandate adoption. In the adjusted analysis, cancer-screening rates were higher among workers residing in exposed MSAs than among those in unexposed MSAs by 1.31 percentage points (95% confidence interval [CI], 0.28 to 2.34) for 12-month colorectal cancer screening, 1.56 percentage points (95% CI, 0.33 to 2.79) for 24-month colorectal cancer screening, 1.22 percentage points (95% CI, -0.20 to 2.64) for 12-month mammography, and 2.07 percentage points (95% CI, 0.15 to 3.99) for 24-month mammography.
CONCLUSIONS: In a sample of private-sector workers in the United States, cancer-screening rates were higher among those residing in MSAs exposed to paid-sick-leave mandates than among those residing in unexposed MSAs. Our results suggest that a lack of paid-sick-leave coverage presents a barrier to cancer screening.
GRANT SUPPORT: R01CA237888/National Cancer Institute
PMID: 36856618
DOI : 10.1056/NEJMsa2209197
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



