Spontaneous Brain Bleeding Might “Spread” with Blood Transfusions!
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
JAMA: Spontaneous Brain Bleeding Might “Spread” with Blood Transfusions!
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
JAMA: Spontaneous Brain Bleeding Might “Spread” with Blood Transfusions!
The analysis of Over a Million Individuals Finds a 173% Increased Risk of Spontaneous Brain Bleeding in Recipients of Multiple Transfusions from Spontaneous Brain Bleeding Patients.
Spontaneous intracerebral hemorrhage (ICH) has various underlying causes.
According to data from a Finnish cohort between 2005 and 2010, approximately 35% of ICH cases can be attributed to high blood pressure, while 20% are associated with cerebral amyloid angiopathy (CAA).
As the second leading cause of ICH, CAA is characterized by the accumulation of misfolded β-amyloid protein (Aβ) in the cerebral cortex and leptomeningeal arteries. CAA exhibits prion-like propagation capabilities, and there is evidence suggesting that Aβ and tau-contaminated pituitary hormones, dural grafts, and potential contamination from neurosurgical instruments can serve as routes for CAA transmission.
Since prions can be transmitted through blood, could blood be one of the pathways for CAA “transmission”?
Recently, scientific teams from Sweden and Denmark conducted a retrospective analysis of data from over a million individuals in their respective countries and found that recipients of blood from individuals who had experienced spontaneous ICH multiple times had a 173% and 132% increased risk of subsequently experiencing spontaneous ICH, respectively.
This suggests that some factor related to blood transfusion might carry a risk for spontaneous ICH.

According to the research data, the risk of recurrent CAA-related brain bleeding is over seven times higher compared to non-CAA-related brain bleeding. Therefore, the researchers considered spontaneous ICH cases in the cohort as either single occurrences or multiple occurrences and used multiple ICH occurrences as a more reliable indicator of CAA. (Hereinafter, all references to ICH refer to spontaneous ICH).
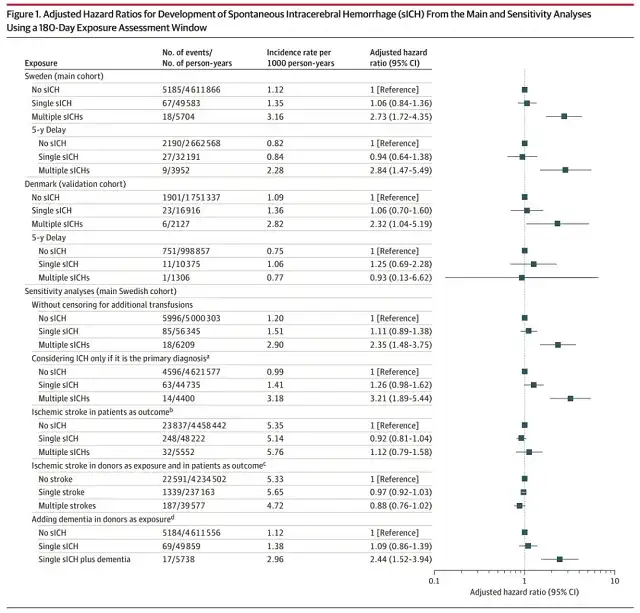
The assumed exposure window for the study was 180 days after receiving a blood transfusion, stratified by donors who had experienced multiple ICH, donors who had experienced a single ICH, and donors who had not experienced ICH before donating blood.
The primary outcome of the study was the occurrence of single or multiple ICH in blood recipients, and the researchers also assessed ischemic stroke as a control, which is another risk factor for ICH.
The Swedish and Danish cohorts included 759,858 and 329,512 participants, totaling over 1.08 million individuals. In the cohorts, 59% and 58% were female, with median ages of 65 and 64 years, respectively.
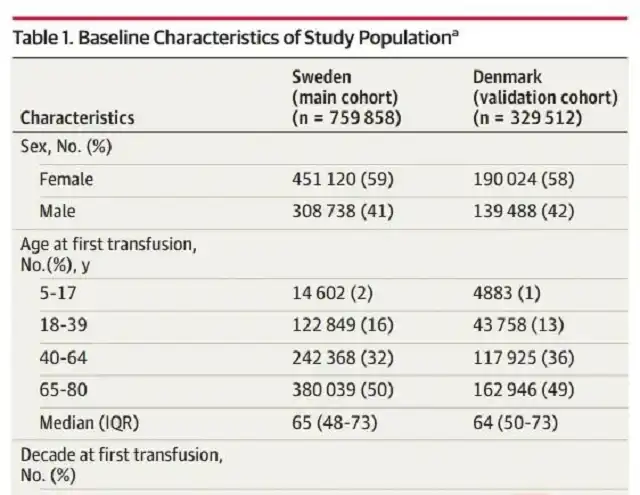
Population baseline characteristics (part)
In both cohorts, approximately 1.1% of participants received blood from donors who had experienced a single ICH, and approximately 0.1% received blood from donors who had experienced multiple ICH.
In the Swedish cohort, it was observed that participants who received blood from donors with multiple ICH occurrences had a significantly increased risk of developing ICH compared to those who received blood from donors without ICH (unadjusted incidence rate of 3.16 vs. 1.12 per 1000 person-years), with a relative risk increase of 173%.
A similar observation was made in the Danish cohort, with incidence rates of 2.82 vs. 1.09 per 1000 person-years and a relative risk increase of 132%.
No association between blood transfusion and ICH was found among participants who only had a single ICH occurrence, and no significant correlation was observed when ischemic stroke was considered as an outcome.
However, in this study, the use of multiple ICH as a surrogate marker for CAA did not provide direct neuropathological or neuroimaging evidence and did not reveal a clear causal relationship. Further research is needed to investigate whether blood transfusion plays a role in CAA transmission and can explain the associations observed in the cohorts.
Reference:
[1] https://jamanetwork.com/journals/jama/article-abstract/2809417
[2] https://jamanetwork.com/journals/jama/article-abstract/2809443
JAMA: Spontaneous Brain Bleeding Might “Spread” with Blood Transfusions!
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



