Johns Hopkins University: Early Plasma Therapy Reduces Long COVID Risk
- Oregon Reverses Course: From Decriminalization to Recriminalization of Drug Possession
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
Johns Hopkins University: Early Plasma Therapy Reduces Long COVID Risk
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Johns Hopkins University: Early Plasma Therapy Reduces Long COVID Risk
A study led by Johns Hopkins University has found that early treatment using plasma from COVID-19 survivors can reduce the risk of “Long-COVID,” with the pro-inflammatory cytokine interleukin-6 (IL-6) playing a critical role in symptom development.
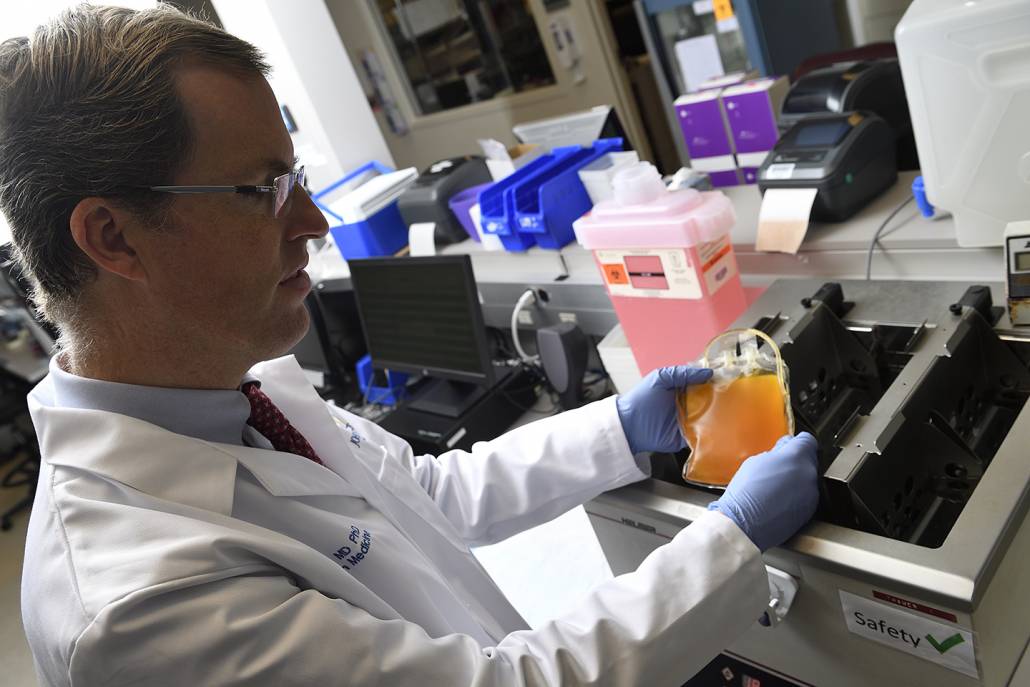
Dr. Aaron Tobian of the Johns Hopkins University School of Medicine thaws a bag of convalescent plasma rich in antibodies collected from COVID-19 patients. A new study led by Johns Hopkins University, with Dr. Tobian as one of the authors, suggests that early treatment using convalescent plasma can lower the risk of COVID patients developing long-term symptoms. Source: Will Kirk, Johns Hopkins University
A nationwide multicenter study led by the Johns Hopkins University School of Medicine and the Bloomberg School of Public Health has shown that COVID-19 patients who receive early plasma therapy from convalescent COVID patients have a reduced risk of developing post-COVID symptoms, commonly referred to as “Long COVID,” as these patients’ plasma contains antibodies against SARS-CoV-2, the virus causing COVID-19.
This new study was first published online on September 19th in the journal “mBio” of the American Society for Microbiology and serves as a follow-up investigation to a clinical trial conducted in 2021, which demonstrated that convalescent plasma as an early outpatient treatment for COVID-19 is an effective and safe option. The latest research examined the long-term effectiveness in most participants from the 2021 clinical trial.
“After our initial study, healthcare professionals began storing plasma rich in SARS-CoV-2 antibodies in their blood banks as a treatment option against COVID-19 for immunocompromised individuals. Now, our new findings suggest that it can also reduce the risk of post-COVID symptoms,” said Dr. David Sullivan, a co-first author of the study and a professor of Molecular Microbiology and Immunology at the Bloomberg School of Public Health and an Infectious Diseases professor at the Johns Hopkins University School of Medicine.
The initial outpatient early treatment clinical trial took place from June 2020 to October 2021. Researchers provided convalescent high-titer plasma (a concentrated mixture containing SARS-CoV-2-specific antibodies) or placebo control plasma (lacking SARS-CoV-2 antibodies) to 1,181 randomly assigned participants. Participants were 18 years and older and tested positive for SARS-CoV-2 within eight days before transfusion. A successful outcome was defined as not requiring hospitalization within 28 days after transfusion.
The initial clinical trial found that among 592 participants who received convalescent plasma, 17 individuals (2.9%) required hospitalization within 28 days after transfusion, whereas among 589 participants who received placebo control plasma, 37 individuals (6.3%) required hospitalization. This indicated a 54% reduction in the relative risk of hospitalization.
As part of the clinical trial, 882 participants underwent screening and assessment of 21 different cytokine and chemokine levels 14 days and 90 days after receiving convalescent or placebo control plasma. Cytokines and chemokines are signaling proteins secreted by cells in response to infection and can activate specific immune system functions, such as inflammation. Excessive or unregulated inflammation is also considered a key factor in triggering post-COVID symptoms.
In the latest study, researchers used measurements of cytokines and chemokines, along with patient reports of any post-COVID symptoms at the 90-day checkup, to determine whether there was an association between early convalescent plasma therapy and long-term COVID symptoms. Statistical analyses were conducted to validate the findings after adjusting for other factors that could make individuals more susceptible to post-COVID symptoms, such as demographic factors (like age and race), comorbid conditions (like diabetes), and vaccination status.
After receiving convalescent or control plasma for 90 days, 590 participants (66.9%) did not experience post-COVID symptoms, while 292 participants (33.1%) reported post-COVID symptoms. The most common symptoms among the latter group were fatigue and loss of smell.
Dr. Aaron Tobian, a senior author of the study and the Director of the Division of Transfusion Medicine at the Johns Hopkins University School of Medicine and a professor of Pathology, stated, “Most study participants had elevated levels of cytokines and chemokines at the screening, and those who received convalescent plasma experienced a greater decrease in cytokine and chemokine levels at day 90. Additionally, participants with elevated levels of interleukin-6 (IL-6) at screening were more likely to experience post-COVID symptoms at day 90. IL-6 is known to trigger human inflammatory responses.”
Dr. Kelly Gebo, a co-first author of the study and a professor of Medicine at the Johns Hopkins University School of Medicine with a Masters in Public Health, remarked, “Our study indicates for the first time that elevated IL-6 early in infection is associated with post-COVID symptoms. While cytokine levels across the entire study population decreased from infection to day 90, the decrease was more pronounced in individuals who received convalescent plasma early in the disease. Therefore, it appears that sustained elevation of IL-6 during the recovery phase of COVID-19 may lead to post-COVID conditions.”
Gebo suggested that future research could investigate the impact of anti-IL-6 agents in combination with other treatment approaches for outpatient COVID-19 patients.
Johns Hopkins University: Early Plasma Therapy Reduces Long COVID Risk
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



