Could In Vitro Embryo Development Become a Reality?
- FDA Approved Opdualag: The First Immunotherapy Targeting LAG-3
- Cutaneous Reactions Following COVID-19 Vaccination: A Review of the Evidence
- Brief Intermittent Exercise Reduces Heart Disease and Death Risk
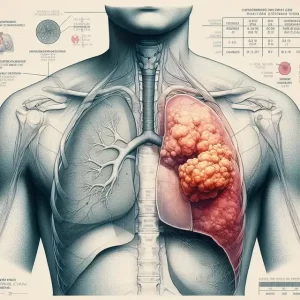
- Personalized Lung Tumor Chips Assess PD-1 Therapy Response
- Study Shows Prior Infection Offers Strong Immunity to Original COVID-19 Strain
- Chinese Food Products Dominate Korean Tables Amid Safety Concerns
Could In Vitro Embryo Development Become a Reality? FDA Evaluates Artificial Womb Technology.
- AstraZeneca Admits for the First Time that its COVID Vaccine Has Blood Clot Side Effects
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Could In Vitro Embryo Development Become a Reality? FDA Evaluates Artificial Womb Technology.
On September 19-20, 2023, the Pediatric Advisory Committee of the United States Food and Drug Administration (FDA) convened a two-day independent advisory meeting to discuss the safety and effectiveness evaluation of Artificial Womb Technology (AWT).
Ethical discussions surrounding the quality of life for premature infants and patient choice took center stage during the meeting.
Attendees expressed that based on current animal data, the technology is not yet ready for human experimentation. “Further research may be needed in more animal models to ensure the safety of this technology and fill in the gaps,” they noted.
The FDA’s Pediatric Advisory Committee, comprised of FDA officials, physicians, industry experts, and patient representatives, met on September 19-20, 2023, to explore ways to better assess the safety and effectiveness of Artificial Womb Technology (AWT). Discussion topics included the limitations of current animal data and the ethical challenges of conducting human trials. Plans for future human trials have not been disclosed as of yet.
Currently, Artificial Womb Technology aims to save the lives of extremely premature infants born before 28 weeks, who have a very low survival rate.
According to a 2022 study published in the Journal of the American Medical Association (JAMA) involving 10,877 infants, the survival rate for infants born at 28 weeks of gestation is 94%, while those born at 23 weeks have about a 50% chance of survival, and at 22 weeks, only 10% can survive. The Centers for Disease Control and Prevention (CDC) reported a 4% increase in premature birth rates between 2020 and 2021. In China, premature birth is defined as the birth of a live infant before 37 weeks of gestation, accounting for about 7% of newborns. Premature birth has become a leading cause of neonatal mortality.
Artificial wombs can replicate the uterine environment, allowing premature infants to continue developing within them and pass through the critical period. Several research groups worldwide are working on developing artificial wombs, with the “BioBag” system developed by Dr. Alan Flake’s team at the Children’s Hospital of Philadelphia (CHOP) being the closest to human experimentation.
On September 14, an article in Nature titled “Human Trials of Artificial Wombs May Start Soon” mentioned CHOP’s case. Researchers at CHOP are seeking approval for their first human clinical trial, which is one of the reasons for the FDA’s independent advisory meeting.
The “BioBag” is a bag filled with sterile fluid that can encase the fetus and provide oxygen and nutrients through tubes. In 2017, this system enabled the survival of a lamb for four weeks. Subsequently, the research team tested their device on pigs and transformed the research into a well-funded startup called Vitara Biomedical, which has raised over $100 million.

The artificial uterus “biobag” developed by CHOP kept a premature lamb alive for four weeks. Image source: “Nature”
Limitations of Animal Experiment Data
Recently, Dr. Alan Flake admitted, “There’s no perfect animal model.” FDA veterinary medical officer Annabelle Crusan explained that fetal sheep are the most commonly used animals for neonatal research because their weight and organ size are similar to human fetuses. However, sheep and humans have different rates of growth. While primates’ fetal growth rates are closest to those of humans, primate fetuses are small, making it difficult to insert them into veins and connect them to machines.
Pigs, on the other hand, have a similar size to human fetuses, but their blood flow differs from that of humans. A team at The Hospital for Sick Children in Toronto, led by Dr. Mike Seed, used pigs for research but has not succeeded in keeping pig fetuses alive for more than one day. Dr. Alan Flake mentioned that his team has attempted pig models but declined to provide detailed experimental data.
“How do we replicate the human uterine environment in terms of growth and nutrition?” asked Dr. Christine Gleason, a pediatric professor at the University of Washington. “I think we need to understand more in animal studies about what we might be overlooking.” Attendees also expressed that based on current animal data, this technology is not yet ready for human experimentation.
“It may require more research in various animal models to ensure the safety of this technology and fill in the gaps,” commented Annabelle Crusan.
Ethical Concerns of In Vitro Embryo Development
Dr. Mark Mercurio, a professor of pediatric ethics and biomedical ethics at Yale University, raised various ethical questions that need to be answered before conducting clinical trials. He pointed out that survival data for premature infants varies among countries and even among different academic centers in the United States. Researchers will have to decide which survival data to consider to identify which fetuses are at the highest risk and determine the suitability of the technology.
“It’s crucial to identify the target population, and it can’t be solely based on gestational age. Other factors also influence fetal survival,” said Mark Mercurio. “In the future, we may be asked by parents if this technology can be used for their child. We need to prepare ethically defensible answers.”
Dr. Mark Mercurio called for a national conference where experts can discuss all the inherent ethical issues of artificial wombs, including how to refer to patients placed in this technology, as they are neither entirely fetuses nor babies.
In the context of the United States, the definition of a fetus is a crucial element of reproductive ethics discussions. For example, in the highly politicized abortion debate in the United States, anti-abortion advocates argue that a fetus is a person from the moment of conception, making abortion the killing of an innocent person unethical. Pro-choice abortion rights advocates emphasize a woman’s bodily autonomy. Even if a fetus is considered a person from the moment of conception, a woman’s bodily autonomy—the right to decide what happens inside and to her body—means that removing the fetus from her body is morally acceptable.
To strike a balance between a woman’s bodily autonomy and the moral status of the fetus, many countries’ abortion laws use “viability” (the fetus’s ability to survive outside the womb, including with medical assistance) as a standard for measuring the ethical acceptability of abortion. In many places where abortion is allowed, a fetus’s right to life surpasses a woman’s bodily autonomy when the fetus becomes capable of independent survival. For example, in the UK, abortion is allowed only up to 24 weeks of gestation, which is currently the earliest developmental stage at which a fetus can survive with medical assistance. The advent of artificial wombs may change this standard, leading to more ethical and legal debates.
During the FDA meeting mentioned above, the quality of life for premature mother-infant pairs and patient choice were central ethical topics. Committee members unanimously agreed that the ultimate goal should not only be survival but also the long-term quality of life for the children. Dr. Charleta Guillory, a pediatric professor at Baylor University, emphasized the high rates of premature births among Black patients and called for a focus on long-term care in the face of health disparities. Committee members also suggested that researchers monitor several potential adverse events, including growth failure, infections, and mother-infant mortality.
Charleta Guillory also stressed the importance of involving a neutral third party in obtaining informed consent from patients: “We need a better assessment system that allows patients to participate in decision-making.” Patient-family representative Gianna McMillan talked about her experience of having to choose between experimental and standard treatments for her child’s malignant brain tumor. She
stated that providing easily understandable information, multiple opportunities for questions, third-party involvement, and ongoing emotional support would be crucial.
“I don’t want people to feel that just because premature birth is complicated and parents are in a difficult situation, they can’t make informed decisions,” said Gianna McMillan.
Could In Vitro Embryo Development Become a Reality? FDA Evaluates Artificial Womb Technology
References:
1. Pediatric Advisory Committee Meeting Announcement, https://www.fda.gov/advisory-committees/advisory-committee-calendar/pediatric-advisory-committee-meeting-announcement-09192023
2. Artificial wombs, after years in development, reach FDA review for human trials, https://www.statnews.com/2023/09/19/fda-studies-artificial-womb-technology/
3. Artificial womb sustains premature baby lambs for weeks, https://www.statnews.com/2017/04/25/mechanical-womb-premature-infant/
4. Artificial Wombs Will Change Abortion Rights Forever, https://www.wired.com/story/ectogenesis-reproductive-health-abortion/
Could In Vitro Embryo Development Become a Reality?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.