Implanting Neural Prostheses Improves Mobility in Parkinson’s Disease Patients of 30 Years
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
Nature Medicine: Implanting Neural Prostheses Improves Mobility in Parkinson’s Disease Patients of 30 Years
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Nature Medicine: Implanting Neural Prostheses Improves Mobility in Parkinson’s Disease Patients of 30 Years
As far back as 30 years ago, there were preclinical and clinical studies indicating that epidural electrical stimulation (ESS) on the lumbosacral spinal cord could restore walking abilities in patients with spinal cord injuries.
However, this required the assistance of several physical therapists, months of intense training, and had very limited success cases. Transforming these complex and rare cases into a widely applicable treatment method has been a massive challenge.
In recent years, Dr. Grégoire Courtine from the Swiss Federal Institute of Technology in Lausanne and neurosurgeon Dr. Jocelyne Bloch from Lausanne University Hospital have developed this technique, which uses epidural electrical stimulation (EES) to reactivate spinal cord neurons, helping dozens of completely paralyzed spinal cord injury patients regain independent mobility.
On November 6, 2023, Dr. Grégoire Courtine, Dr. Jocelyne Bloch, and others published a research paper titled “A spinal cord neuroprosthesis for locomotor deficits due to Parkinson’s disease” in the prestigious medical journal Nature Medicine.
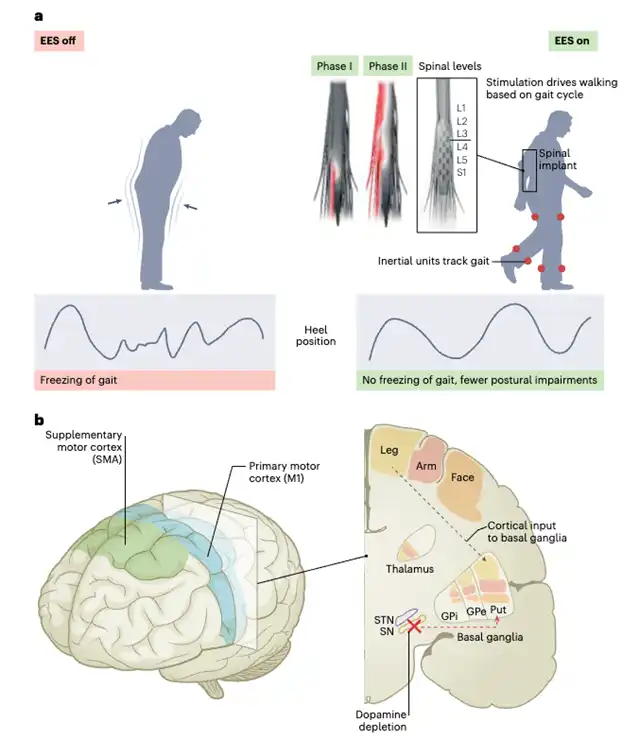
This study utilized targeted epidural electrical stimulation through the implantation of a neural prosthesis to improve the walking and balance capabilities of a person severely affected by Parkinson’s disease. The research highlights the potential of using neural prosthetic devices to treat movement disorders in Parkinson’s disease patients.

Approximately 90% of advanced Parkinson’s disease patients experience mobility issues, including gait disturbances, balance problems, and freezing of gait episodes. These challenges significantly reduce their quality of life and the severity of related conditions, and existing therapies are often ineffective. Targeted epidural electrical stimulation (EES) of the lumbosacral spinal cord can modulate neural activity controlling movement. Recent studies have shown that this technology can restore standing and walking abilities in paralyzed individuals due to spinal cord injuries.
In this study, Dr. Grégoire Courtine and his team developed a neural prosthesis based on epidural electrical stimulation (EES) to restore the natural activation of leg nerves disrupted during walking in Parkinson’s disease patients.
Following extensive validation of the neural prosthesis using non-human primate models, the research team initiated the first human trial of this approach. The trial involved a 62-year-old male who had suffered from Parkinson’s disease for 30 years, experiencing severe mobility issues despite previous treatments, including medication and deep brain stimulation.
The research team first created a customized anatomical map for EES targeting in the lumbosacral spinal cord region, guiding the precise surgical implantation of the neural prosthesis. Subsequently, wireless sensors worn by the patient detected his movement intentions, triggering EES to activate the leg nerves and generate natural walking movements.
The results of the study indicated that the implanted neural prosthesis improved the participant’s walking and balance difficulties, leading to a significant enhancement in his quality of life. The patient has now been using the prosthesis for two years, approximately 8 hours per day.
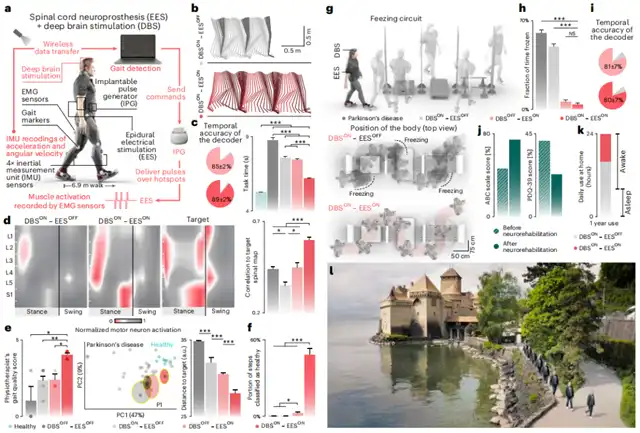
The neural prosthesis alleviated gait disturbances, balance issues, and the frequency of freezing of gait in Parkinson’s disease patients, enhancing their quality of life and supporting their mobility in community settings.
These preliminary findings suggest that targeted EES may be a promising treatment option for common mobility issues in Parkinson’s disease patients. However, this is a proof-of-concept study with only one participant, and further research is needed in larger clinical trials to validate the effectiveness of this approach.
For further reading:
In October 2018, Dr. Grégoire Courtine and Dr. Jocelyne Bloch developed a targeted neural technology using epidural electrical stimulation (EES) to reactivate spinal cord neurons, enabling three chronic paraplegic patients to regain the ability to walk. This study was published as a cover article in the journal Nature.
In February 2022, the team published a paper in Nature Medicine introducing a personalized spinal cord stimulation electrode controlled by artificial intelligence software. After implantation, this electrode activates the spinal cord regions responsible for trunk and leg muscle control, allowing three completely paralyzed spinal cord injury patients to regain independent mobility within hours, including the ability to stand, walk, ride a bicycle, swim, and control trunk movements.
In November 2022, the team published a paper in Nature, demonstrating the successful recovery of walking abilities in nine patients with severe or complete paralysis due to spinal cord injuries using epidural electrical stimulation (EES). The study also elucidated the critical role played by specific neuron types in the spinal cord neuronal remodeling process, contributing to a deeper understanding of how mobility can be restored after paralysis.
In May 2023, the team published a paper in Nature introducing a brain-spinal cord interface (BSI) that connects the brain to the spinal cord region responsible for walking.
This device can be calibrated within minutes and offers reliable and stable operation for over a year. The BSI successfully helped chronic quadriplegic patients control leg movements for standing, walking, climbing stairs, and navigating complex terrain.
Importantly, this BSI-supported neural rehabilitation promotes neural recovery, allowing patients to regain the ability to walk with the use of crutches even when the BSI is turned off. This concept of building a digital bridge between the brain and the spinal cord may have implications for improving the treatment of movement disorders caused by neurological diseases.
Nature Medicine: Implanting Neural Prostheses Improves Mobility in Parkinson’s Disease Patients of 30 Years
Papers Links:
1. https://www.nature.com/articles/s41591-023-02584-1
2. https://www.nature.com/articles/s41586-018-0649-2
3. https://www.nature.com/articles/s41591-021-01663-5
4. https://www.nature.com/articles/s41586-022-05385-7
5. https://www.nature.com/articles/s41586-023-06094-5
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



