Quadrupled Survival: Localized Treatment Breakthrough in Metastatic Cancers
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Quadrupled Survival: Localized Treatment Breakthrough in Metastatic Cancers
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Quadrupled Survival: Localized Treatment Breakthrough in Metastatic Cancers.
Significant Progress: Survival Period Extended Over 4 Times! “The Lancet” Highlights Localized Treatment for Metastatic Cancer.
Oligoprogression, defined as a state between limited and widespread metastatic cancer with a few metastases in specific organ sites, poses a unique challenge in treatment. Most patients with metastatic cancer eventually develop resistance to systemic therapies. However, recent clinical research indicates that patients with oligoprogression, characterized by a limited number of metastases, may benefit from localized treatments such as surgery or radiotherapy.
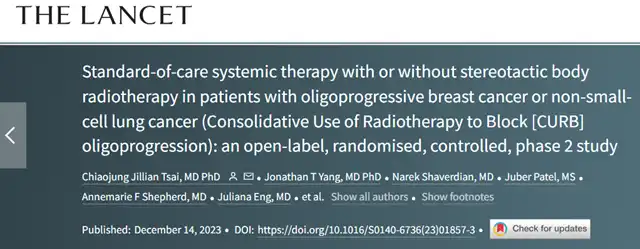
A recent phase 2, randomized controlled study published in “The Lancet” suggests that targeted treatment using stereotactic body radiotherapy (SBRT) on oligoprogressive lesions can improve patient outcomes.
Data analysis reveals that, compared to standard treatment, SBRT combined with standard treatment significantly prolongs the progression-free survival (PFS) of patients with oligoprogressive cancer.
Notably, non-small cell lung cancer (NSCLC) patients who received SBRT in addition to standard treatment experienced a PFS extension of over four times compared to those receiving standard treatment alone.
Researchers conducted a phase 2, open-label, randomized controlled trial to assess the efficacy of SBRT in patients with oligoprogressive metastatic breast cancer or NSCLC, who had at least received first-line systemic treatment. Oligoprogression was defined as the presence of ≤5 progressing lesions based on PET-CT or CT scans.
Patients were randomly assigned to receive either standard treatment (standard treatment group) or SBRT combined with standard treatment (SBRT group) in a 1:1 ratio. Patient stratification was based on factors such as the number of metastases, receptor or driver gene mutation status, primary site, and previous systemic treatment type. The primary endpoint of the study was PFS.
Between January 1, 2019, and July 31, 2021, a total of 106 patients were randomly assigned to the standard treatment group (n=51, including 23 breast cancer and 28 NSCLC patients) or the SBRT+standard treatment group (n=55, including 24 breast cancer and 31 NSCLC patients).
Among the 47 breast cancer patients, 16 (34%) had triple-negative breast cancer, and among the 59 NSCLC patients, 51 (86%) did not have targetable driver mutations. The median follow-up times for the standard treatment and SBRT+standard treatment groups were 11.6 months and 12.1 months, respectively.
Analysis results showed that the median PFS for the standard treatment group was 3.2 months, while the SBRT+standard treatment group had a median PFS of 7.2 months (HR=0.53; 95% CI 0.35~0.81; p=0.0035). Specifically, NSCLC patients in the SBRT+standard treatment group had significantly higher median PFS compared to NSCLC patients in the standard treatment group (10.0 months vs. 2.2 months; HR=0.41; 95% CI 0.22~0.75; p=0.0039). However, there was no significant difference in the median PFS between breast cancer patients in the SBRT+standard treatment group and the standard treatment group (4.4 months vs. 4.2 months; HR=0.78; 95% CI 0.43~1.43; p=0.43).
In terms of safety, 21 patients (41%) in the standard treatment group and 34 patients (62%) in the SBRT+standard treatment group experienced ≥grade 2 adverse events. Among these, 9 patients (16%) in the SBRT+standard treatment group had ≥grade 2 SBRT-related toxic events, including gastroesophageal reflux disease, increased pain, radiation pneumonitis, brachial plexopathy, and decreased blood cell count.
In conclusion, the analysis of this trial’s results suggests that, compared to receiving standard treatment alone, SBRT+standard treatment can extend the PFS of patients. Oligoprogressive metastatic NSCLC patients can benefit significantly from SBRT+standard treatment, with a PFS extension of over four times compared to standard treatment alone.
Quadrupled Survival: Localized Treatment Breakthrough in Metastatic Cancers
Reference:
Standard-of-care systemic therapy with or without stereotactic body radiotherapy in patients with oligoprogressive breast cancer or non-small-cell lung cancer (Consolidative Use of Radiotherapy to Block [CURB] oligoprogression): an open-label, randomised, controlled, phase 2 study. THE LANCET. DOI: 10.1016/S0140-6736(23)01857-3
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



