FDA and US Military at Odds Over Quality of Indian Generic Drugs?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
FDA and US Military at Odds Over Quality of Indian Generic Drugs?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
FDA and US Military at Odds Over Quality of Indian Generic Drugs?
1. Outrage in the U.S. Military as Inferior Indian Generic Drugs Cause Concerns
The U.S. military has openly expressed anger over safety issues related to substandard generic drugs, prompting the Pentagon to seek assistance from independent laboratories for the analysis of certain critical medications.
The FDA’s reluctance to address the military’s concerns and its inaction in drug quality testing have exacerbated the severity of the problem.
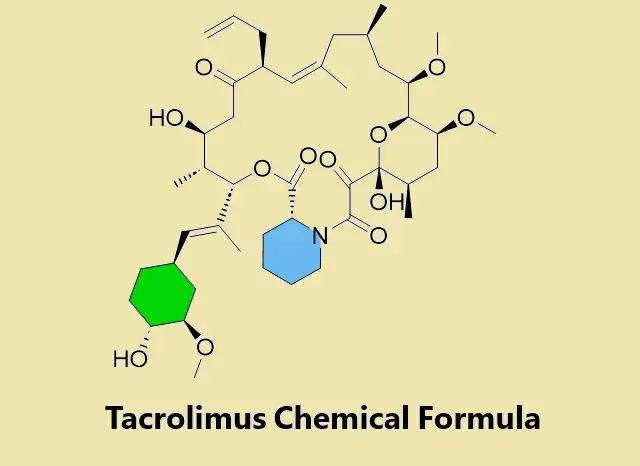
For an extended period, some doctors have been warning the FDA about the subpar efficacy of certain generic versions of Tacrolimus, an immunosuppressive drug used to reduce the risk of rejection after organ transplantation.
However, it was discovered that some inferior generic versions of Tacrolimus could potentially lead to kidney failure and seizures. Independent labs entrusted by the U.S. military to examine Tacrolimus found that the version manufactured by India’s Intas Pharmaceuticals Ltd was not equivalent to the brand-name drug.
The quality issues with Tacrolimus are just the tip of the iceberg in the crisis exposed by the military’s concerns.
2. Proliferation of Issues in Indian Pharmaceutical Manufacturing
While cheap generic drugs save the U.S. billions annually, they also create significant challenges. From 2018 to 2022, recalls related to drug manufacturing quality in the U.S. doubled, with nearly 80% of FDA-registered generic drug manufacturing facilities located overseas.
The profit margins for generic drugs are typically low, leading to a situation where only one or two suppliers may provide crucial medications. This quality issue is exacerbating severe shortages in the drug supply chain. The U.S. is experiencing near-historic levels of drug shortages this year, affecting cancer patients desperately in need of life-saving medications. While affordable generic drugs are crucial for the entire healthcare system, safety concerns have become a significant Achilles’ heel for generic drugs.
In February of this year, the U.S. health authorities detected rare antibiotic-resistant bacteria, Pseudomonas aeruginosa, in eye medications produced in India. The outbreak resulted in four deaths, several cases of blindness, and infections in the U.S. These eye drops were sold over the counter in major U.S. pharmacies and originated from a factory that had never undergone FDA inspection. An investigation by Bloomberg revealed that this outbreak was undoubtedly a result of regulatory loopholes in the FDA, allowing many over-the-counter drugs, including sensitive medications requiring sterility, to enter the U.S. market without inspection. Over the past year and a half, cough syrups manufactured in India containing toxic industrial solvents (ethylene glycol and diethylene glycol) have led to at least 140 child deaths in 10 countries, including The Gambia and Uzbekistan.
With the ongoing “de-Chinafication” in the U.S., reliance on Indian manufacturers is increasing. However, in the process of seeking a “strategic partnership,” the FDA’s actions to address defective drugs have been slow. Last month, U.S. media reported that eye drops removed from pharmacy shelves across the U.S. were produced in an unsanitary factory in India, where workers operated barefoot and falsified test results. The eye drops were manufactured by Kilitch Healthcare India Ltd. in Navi Mumbai, India, and their products had entered the marketplaces of major U.S. retailers such as Walmart Inc., CVS Health Corp., and Target Corp.
According to the FDA database, their inspectors visited Kilitch’s facility in mid-October. Shortly after a seven-day inspection, the FDA issued a warning, stating that the eye drops could potentially cause partial vision loss or blindness. The FDA, at that time, did not mention Kilitch’s name in their warning report. Still, Bloomberg identified the company through inspection reports. The FDA almost lacked the authority to mandate a recall of Kilitch’s products but did, on October 23, prohibit Kilitch’s factory from exporting more eye drops to the U.S. Two days later, the FDA requested the company to recall its products, a request that Kilitch refused.
In an email statement, an FDA spokesperson expressed their active collaboration with retailers to remove these products from shelves and urged consumers to stop using them due to the risk of eye infections. The inspection report revealed that FDA inspectors observed workers in the sterile area not wearing proper protective gear. One employee even removed a hat and combed their hair while handling cleaning equipment. Inspectors also observed testing personnel falsifying retrospective test results, claiming that the results indicated the batch of eye drops was sterile. Samples collected during the inspection showed bacterial contamination in the bottling area of the eye drops.
Rebecca Petris, chair of the Dry Eye Foundation, stated that this year’s recall incidents left consumers “confused and scared.” The Dry Eye Foundation is a non-profit organization based in the suburbs of Seattle that issues safety recommendations for eye drops. The organization noted that the FDA has publicly warned consumers about 78 non-prescription eye drops this year, but only 13 have been recalled.
The FDA examined 163 drugs that faced shortages from 2013 to 2017, and the results indicated that quality issues were the absolute leading cause of drug shortages.
3. Pentagon Seeks Help from Independent Labs; FDA Expresses Displeasure
Concerns about the national drug supply prompted the Pentagon in August of this year to choose an independent laboratory, Valisure LLC, with whom the FDA openly disagreed. The laboratory was commissioned to test the quality of certain generic drugs that millions of military personnel and their families might use. Two years ago, the U.S. military also chose the healthcare system Kaiser Permanente for similar investigative activities.
Although the FDA’s mission includes controlling the quality of drugs, the actions of the U.S. military have shown friction between the two organizations. In fact, the FDA has resisted the idea of grading drugs based on quality and rarely conducts its testing. Several U.S. government officials have indicated that the FDA attempts to block the Pentagon from intervening, questions Valisure’s methods, and impedes broader efforts by the U.S. government this year to introduce third-party testing more extensively. However, continuous revelations of drug quality scandals in India, especially practices challenging the bottom line by pharmaceutical companies like Intas, have made the FDA uneasy. Despite the FDA banning Intas from exporting certain products to the U.S. market, the ban grants a “get out of jail free card” to over 20 generic drugs (including Tacrolimus and 16 cancer drugs).
The issue of Indian drugs has a long history. In 2013, the U.S. subsidiary of India’s Ranbaxy Laboratories Ltd. shocked the generic drug market by admitting to selling adulterated drugs and lying to the FDA. Ranbaxy settled the case by paying $500 million, but this scandal further exposed the deficiencies in the FDA’s overseas inspection system. While surprise inspections are easily conducted in the U.S., overseas inspectors often need to announce their visits five days in advance.
In 2014, the second year after the Ranbaxy incident, the FDA initiated a surprise inspection pilot program in India, unsurprisingly discovering more issues. The inspected facilities were not only dirty and lacked equipment, but staff also frequently hid sensitive documents. However, this inspection pilot program ultimately “fizzled out” without a clear explanation from the FDA. According to former FDA insiders, surprise inspections might jeopardize efforts to deepen relations with India. This was around the time when Modi had been in office for just over a year.
According to Bloomberg’s2020 report, the FDA’s risk-based inspection program had been abused by Indian pharmaceutical companies. The program allowed the FDA to only inspect facilities based on potential risks, but companies anticipated this approach and concealed issues. Surprisingly, several generic drug manufacturing facilities in India escaped FDA inspections for nearly a decade.
This year’s emergence of an Indian generic version of Tacrolimus that could potentially lead to kidney failure and seizures has rekindled concerns about the FDA’s inspections in India. The issue also reflects on the FDA’s shortcomings in handling quality control matters. While generic drugs significantly reduce healthcare costs, the FDA’s inadequate response to safety concerns and quality control issues poses a considerable risk to public health, particularly among military personnel who depend on these medications.
4. Conclusion: Balancing Affordability and Safety
The ongoing crisis surrounding generic drugs manufactured in India highlights the urgent need for a comprehensive solution that balances the affordability of medications with rigorous safety standards. The U.S. military’s concerns, backed by independent laboratory testing, shed light on the potential risks associated with certain generic drugs, emphasizing the importance of robust quality control measures.
While the affordability of generic drugs is crucial for managing healthcare costs, compromising on safety can lead to severe health consequences. The FDA plays a central role in ensuring the safety and efficacy of medications, and it is imperative for the agency to address the challenges posed by substandard generic drugs.
Moving forward, a collaborative approach involving regulatory bodies, pharmaceutical companies, and independent laboratories is essential to establish a more robust system for monitoring and ensuring the quality of generic drugs, especially those manufactured overseas. Striking a balance between affordability and safety is paramount to safeguarding public health and maintaining trust in the pharmaceutical industry.
As the U.S. grapples with the complexities of its drug supply chain and increasing reliance on generic medications, policymakers, healthcare professionals, and regulatory agencies must work together to implement effective measures that prioritize both accessibility and safety in the pharmaceutical landscape.
FDA and US Military at Odds Over Quality of Indian Generic Drugs?
References:
1.Mider, Z. et al. Poisoned Cough Syrup Killed Kids. Authorities Cut the Investigation Short. Bloomberg. 11. 07. 2023.
2.Snider, M. Recalled contaminated eye drops linked to bacteria have led to a fourth death, CDC says. US Today. 20. 05. 2023.
3.Edney, A. et al. Tainted Walmart, CVS Eyedrops Tied to Unsanitary Indian Factory. Bloomberg. 10 .11. 2023.
4.Robinson, P. et al. No Testing, No Inspections: Contaminated Eyedrops Blinded and Killed Americans. Bloomberg. 18. 07. 2023.
5.New Survey: 1 in 10 Cancer Patients Has Been Impacted by Nation’s Drug Shortages with Significant Delays to Cancer Care. American Cancer Society Press Release. 19. 10. 2023.
6.E&C Republicans Press FDA Over Inadequate Inspection of Drug Manufacturing in India and China. 18. 07. 2023. https://energycommerce.house.gov/posts/e-and-c-republicans-press-fda-over-inadequate-inspection-of-drug-manufacturing-in-india-and-china#
7.Mider, Z. Iraqi Government Recalls Tainted Cold Medicine Made in India. Bloomberg. 02. 08. 2023.
8.OMCL – Background and mission. Council of Europe. Retrieved on 10. 12. 2023.
9.Edney, A. et al. The Pentagon Wants to Root Out Shoddy Drugs. The FDA Is In Its Way. Bloomberg. 05. 12. 2023.
(source:internet38SIYS6bDe7aB6DwVPXt6g, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



