Why are more and more young people getting cancer?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Why are more and more young people getting cancer?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Why are more and more young people getting cancer?
In some countries, including the United States, the cancer death rate is declining due to increased screening, decreased smoking rates, and new treatment options. However, globally, the incidence of cancer is on the rise.
Early-onset cancers—typically defined as cancers that occur in adults under the age of 50—still account for only a small fraction of total cases, but the incidence has been increasing.
This growth, coupled with the increase in the global population, has led to a nearly 28% rise in global early-onset cancer deaths from 1990 to 2019. Models also suggest that the death rate may continue to rise.
Typically, these early-onset cancers affect the digestive system, with colorectal, pancreatic, and stomach cancers showing the fastest growth in incidence. Colorectal cancer is one of the most common cancers globally and often garners the most attention. However, other cancers—including breast and prostate cancers—are also on the rise.
In the United States, the data on cancer incidence is particularly stringent, with endometrial cancer increasing by 2% annually in adults under 50 since the mid-1990s. Early-onset breast cancer is increasing by 3.8% between 2016 and 2030.
In the United States, cancer incidence rates are increasing faster in women than in men, and faster in Hispanic populations than in non-Hispanic white populations. The rate of increase in colorectal cancer incidence among young American Indian and Alaska Native individuals is faster than that among white individuals. Compared to white individuals, Black individuals diagnosed with early-onset colorectal cancer are more likely to be diagnosed at a younger age and at a later stage.
Cases of early-onset cancer
Among the many young cancer patients treated by Cathy Eng, one that stood out was a young woman with cancer typically diagnosed at age 65. This 16-year-old girl flew from China to Texas, USA, for treatment of gastrointestinal cancer, which typically occurs in older individuals. Her parents sold their house to fund her care, but it was too late.
“It’s already very advanced,” says Eng, now an oncologist at Vanderbilt University Medical Center in Nashville, Tennessee. “I was powerless.”
Eng specializes in adult cancers. While the Chinese girl she saw a decade ago was the youngest patient Eng had seen with her type of cancer, she wasn’t the only one who seemed too young, too healthy, for the cancer she had.
In Mumbai, India, surgeon George Barreto noticed the same thing. These observations quickly became personal. Friends and family members were also diagnosed with unlikely cancers. “And then I made a mistake that one should never make,” says Barreto (now at Flinders University in Adelaide, Australia). “I promised them that I would find out.”
Candace Henley was diagnosed with colorectal cancer at age 35, a single mother raising five children. The aggressive surgery she underwent left her unable to continue her job as a bus driver, and the family soon became homeless.
Since Eng first noticed her patients being so young, some things have changed. Advocacy groups have started targeting their messaging to younger audiences. Eng says that young-onset cancer patients are now more informed and will switch hospitals if their symptoms are dismissed by doctors. This might mean that doctors are more likely to find early-onset cancers before they spread and become harder to treat (in other words, early-onset cancers that might have gone undetected in the past).
Barreto, Eng, and other oncologists collected data, a commitment that took years to progress. Statistics from around the world now paint a clear picture: the incidence of dozens of cancers is increasing among adults under 50. This growth varies by country and cancer, but based on global data, models predict that the number of early-onset cancer cases will increase by around 30% from 2019 to 2030. In the United States, colorectal cancer—typically occurring in men over 60—has become the leading cause of cancer death in men under 50. In young women, it’s the second leading cause of cancer death.
As calls for better screening, awareness, and treatment grow louder, researchers are racing to explain why incidence rates are rising. The most likely factors—such as increasing obesity rates and early cancer screening rates—do not fully explain this growth. Some are looking at the gut microbiome or the tumor’s own genome for answers. But many believe that the answers to these questions still lie in studies tracking the lives and health of children born half a century ago.
No single study can find the cause; it may be a combination of factors.
Genetic Clues
The prominence of gastrointestinal cancers and changes in the diets of many nations suggest that rising obesity rates and diets rich in processed foods may be the culprits behind the rising incidence. But Daniel Huang, a hepatologist at the National University of Singapore, says that statistical analyses suggest that these factors alone do not fully explain the situation. “Many assume that factors like obesity and alcohol consumption can explain some of our findings. But it looks like you need to dive deeper into the data.”
These analyses align with anecdotal experiences described by clinical doctors to Nature: the young people they treat are typically healthy, look healthy, and have almost no cancer risk factors. A 32-year-old woman treated by Eng was preparing for a marathon. Previous doctors thought her bloody stools were due to irritable bowel syndrome caused by intense training. “She was very healthy,” Eng says. “If you look at her closely, you wouldn’t know that more than half of her liver was tumors.”
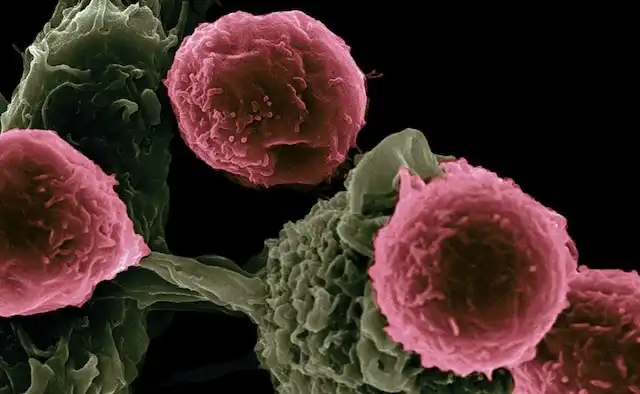
Prominent cancer research funders, including the U.S. National Cancer Institute and the U.K. Cancer Research Institute, are supporting projects to find other factors that may contribute to early-onset cancer. One approach is to look for genetic clues that could differentiate early-onset tumors from those in older adults. Pathologist Shuji Ogino of Harvard Medical School in Boston and his colleagues have identified some possible features of aggressive tumors in early cancer. For example, aggressive tumors are sometimes particularly good at suppressing the body’s immune response to cancer, and Ogino’s research group has found signs of weakened immune responses to some early tumors.
But he says these differences are subtle, and researchers have not yet found a clear boundary between early-onset and late-onset cancers. “It’s not a dichotomy, but more like a continuous spectrum,” he says.
Researchers are also studying the microbiota living inside the body. Disruption of the microbiome composition, such as from dietary changes or antibiotics, is associated with increased risk of inflammation and several diseases (including some forms of cancer). Whether there is a link between the microbiome and early-onset cancer is still a question: so far, results are preliminary, and collecting long-term data is challenging, says Christopher Lieu, an oncologist at the University of Colorado Cancer Center in Aurora. “There are so many factors that affect the microbiome. You ask people to remember what they ate as children, and I can hardly remember what I had for breakfast.”
Tracing Back to the Womb
Finding research from prenatal to adulthood is a challenge. Ogino says that ideally, a study should recruit thousands of expectant mothers across several countries, collect data and samples of blood, saliva, and urine, and then track them for decades. A research group funded by the Cancer Research Institute in the U.K., the National Cancer Institute in the U.S., and other institutions will
in older adults. Her parents sold their house to fund her care, but it was already too late.
“She was already very advanced, and there was nothing I could do,” says Eng, a oncologist at Vanderbilt University Medical Center in Nashville, Tennessee.
Eng specializes in adult cancers. While the Chinese girl she saw a decade ago was her youngest patient, she was not the only one who seemed too young and healthy for the cancer she had.
In Mumbai, India, surgeon George Barreto also noticed the same thing. He says these observations quickly turned into personal observations. Friends and family members were also diagnosed with unlikely cancers. “And then I made a mistake people should never make,” says Barreto (now at Flinders University in Adelaide, Australia). “I promised them that I would investigate thoroughly.”
Candace Henley was diagnosed with colorectal cancer at the age of 35, a single mother raising five children. The intense surgery she underwent left her unable to continue her job as a bus driver, and the family was soon homeless.
Since Eng first noticed her patients were so young, some things have changed. Some advocacy groups have started targeting their messaging to younger audiences. Eng says that early-onset cancer patients are now more aware, and when doctors dismiss their symptoms, they switch hospitals and get reevaluated. This could mean that doctors will more often discover early-onset cancers before they spread and become harder to treat (in other words, early-onset cancers that may have been missed in the past).
Barreto and Eng, along with other oncologists, collected data, a commitment that took years to materialize. Statistics from around the world now make it clear: the incidence of several cancers is increasing among adults under 50. This increase varies by country and cancer, but based on global data, models predict that the number of early-onset cancer cases will increase by around 30% between 2019 and 2030. In the United States, colorectal cancer—typically occurring in men over 60—is now the leading cause of cancer death in men under 50. In young women, it is the second leading cause of cancer death.
As calls for better screening, awareness, and treatment grow louder, researchers are racing to explain why the incidence is rising. The most likely factors—such as rising obesity rates and increased early cancer screening rates—do not fully explain this growth. Some are looking for answers in the gut microbiome or the genomes of the tumors themselves. But many believe the answers to these questions still lie in tracking the lives and health of children born half a century ago.
No single study has found the answer; it may be a combination of different factors.
Genetic clues
The prominence of gastrointestinal cancers and changes in the diets of many nations suggest that the rising obesity rate and diets rich in processed foods may be the main culprits behind the rising incidence. But Daniel Huang, a hepatologist at the National University of Singapore, says that statistical analysis suggests these factors alone are not enough to explain the whole picture. “Many people assume that factors such as obesity and alcohol consumption can explain some of our findings. But it seems that you need to delve deeper into the data.”
These analyses are consistent with anecdotal experiences described by clinicians in Nature magazine: the young people they treat are generally healthy, look healthy, and have almost no cancer risk factors. Eng treated a 32-year-old woman who was preparing for a marathon. Previous doctors thought her bloody stools were caused by irritable bowel syndrome from intense training. “She was very healthy,” Eng says. “If you looked at her closely, you wouldn’t know that more than half of her liver was tumors.”
Prominent cancer research funders, including the National Cancer Institute in the United States and the Cancer Research UK, support projects to find other factors that could lead to early-onset cancer. One approach is to look for genetic clues that could distinguish early-onset tumors from those in older adults. Pathologist Shuji Ogino and his colleagues at Harvard Medical School in Boston, Massachusetts, have identified some possible features of aggressive tumors in early cancer. For example, aggressive tumors are sometimes particularly good at suppressing the body’s immune response to cancer, and Ogino’s research group has found signs of weakened immune response to some early tumors.
But he says these differences are subtle, and researchers have not yet found a clear boundary between early-onset and late-onset cancers. “It’s not a dichotomy; it’s more like a continuous spectrum,” he says.
Researchers are also studying the microbiota living in the body. Disruptions to the microbiome, such as those caused by changes in diet or antibiotics, are associated with an increased risk of inflammation and several diseases (including certain forms of cancer). Whether there is a link between the microbiome and early-onset cancer remains a question: so far, results are preliminary, and it is difficult to collect long-term data, says Christopher Lieu, an oncologist at the University of Colorado Cancer Center in Aurora, Colorado. He says, “The factors affecting the microbiome are very broad. You ask people to recall what they ate as children, and I can barely remember what I had for breakfast.”
Tracing back to the womb
Finding studies from prenatal to adulthood is a challenge. Ogino says the ideal study would recruit thousands of prospective mothers in several countries, collect data and samples of blood, saliva, and urine, and then track them for decades. A research team funded by the Cancer Research UK, the National Cancer Institute, and other institutions will analyze data from the United States, Mexico, and several European countries to identify environmental exposures and other factors that may affect the risk of early-onset cancer. They also hope to include data collected from fathers in the study and analyze blood samples with collaborators to look for more chemicals offspring may encounter in the womb.
Murphy expects the results to be complex. “At first, I really believed that early-onset colorectal cancer had some unique features, and there was one risk factor that explained everything. The longer I spent, the more clear it became that it wasn’t just one thing; it was a bunch of risk factors.”
Irit Ben-Aharon, an oncologist at Rambam Health Care Campus in Haifa, Israel, says that social determinants of health are also likely playing a role in the differences in early-onset cancer. These determinants include access to healthy foods, lifestyle factors, and systemic racism.
Why are more and more young people getting cancer?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



