Therapeutic targeting of hypertension and inflammation
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
Therapeutic targeting of hypertension and inflammation: from a novel mechanism to a transformational perspective.
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Therapeutic targeting of hypertension and inflammation: from a novel mechanism to a transformational perspective.
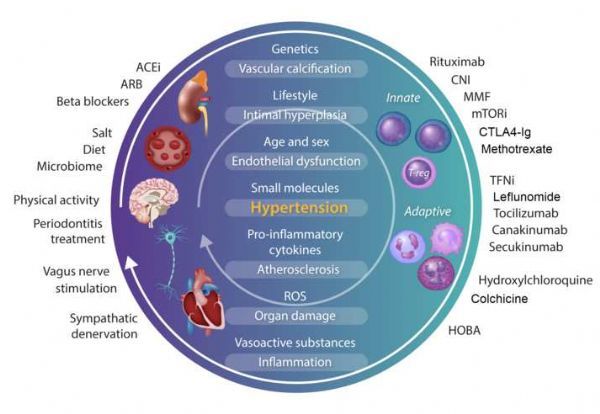
Animal models, human observations and genetic studies have shown that immune and inflammatory mechanisms play a key role in hypertension and its complications. The author reviewed the effects of immunomodulatory interventions on blood pressure, target organ damage, and human cardiovascular risk.
Animal models of human observation and genetic research study showed that the immune and inflammatory mechanisms in hypertension plays a key role and its complications. The author reviewed the effects of immunomodulatory interventions on blood pressure, target organ damage, and human cardiovascular risk.
In experiments and small clinical studies, whether it is non-specific immunomodulatory methods, such as mycophenolate mofetil and methotrexate, or 8 drugs that target T lymphocytes and B lymphocytes , such as tacrolimus and cyclosporine Vitamins, everolimus, and rituximab can lower blood pressure and reduce organ damage.
In many studies, the trial design has become complicated due to the lack of blood pressure-related endpoints, the inclusion of the majority of the normal blood pressure study population, multiple drugs, and established comorbidities. Among a wide range of interventions reviewed, TNF-α inhibitors provide the most powerful evidence for lowering blood pressure.
The treatment of periodontitis also seems to have a non-drug lowering blood pressure effect. Evidence that immunomodulatory drugs affect organ damage mediated by hypertension is discussed.
Animal models, observational studies, and human test data support the therapeutic potential of targeted immunotherapy in reducing blood pressure and organ damage mediated by hypertension . Targeted research is now needed to address their impact on the blood pressure of hypertensive patients.

Image source: https://pubmed.ncbi.nlm.nih.gov/34698811/
In atherosclerosis, the role of inflammation has been clearly defined. In the ESC Cardiovascular Disease Prevention Guidelines, coexisting chronic inflammatory conditions such as rheumatoid arthritis , inflammatory bowel disease, ankylosing spondylitis and psoriasis are considered It is an additional risk factor.
Anti-inflammatory therapy is recommended for these 6 patients. Recent clinical trials such as CANTOS , COLCOT and LoDoCo2 support the improvement of cardiovascular outcomes through inflammation. Hypertension is the most common cardiovascular risk factor.
In recent years, immune cells have been observed to infiltrate the kidneys and blood vessels of hypertensive humans and experimental hypertensive animals. There is increasing evidence that immune and inflammatory mechanisms promote this disease.
Therefore, it is crucial to determine clinically permitted therapeutic interventions to address the inflammatory targets of hypertension and the patient population will benefit from them.
Although basic and translational evidence suggests that intervention in the immune-inflammatory process may help control blood pressure (BP) and prevent target organ damage, the clinical evidence of these interventions has not yet been systematically analyzed.
Therefore, the authors reviewed potential immunotherapy targets to identify methods that may prove effective in well-designed clinical studies.
Inflammation and immune activation were first thought to be related to hypertension, which was first confirmed by Grollman, Okuda, Svensen and Olsen . In the past decade, new research has begun to reveal the mechanism that explains this phenomenon.
Using genetic and pharmacological targeted animal models, the regulatory effects of T cells, cells, monocytes / macrophages, dendritic cells, B cells, NK cells, and other components of the complex immune-inflammatory network were evaluated . The onset of hypertension inflammation seems to be related to oxidative stress and redox-dependent mechanisms in blood vessels and kidney tissues.
These will lead to the generation of new antigens, damage-related molecular patterns (DAMP) and neuroimmune mechanisms, which will trigger a maladaptive immune response, thereby aggravating the damage of hypertension and its related organs.
Although the antigen that activates adaptive immunity has not yet been determined, a potential candidate protein is isolevugandin (isoLG) adduct protein. isolg is the oxidation product of arachidonic acid, which can quickly connect from the lysine on the protein, accumulate in the antigen-presenting cells, and present in the major histocompatibility complex. They activate a subset of CD4+ and CD8+ T cells.
Importantly, the isoLG selective scavenger 2 -hydroxybenzylamine (2-HOBA) can prevent immune activation and lower blood pressure in several animal models of hypertension.
Data from animal and human studies also confirm that HSP70 is a potential autoantigen. In a wide range of models, a large number of animal studies have emphasized that the immune regulation of inflammatory activation and the release of effector cytokines may suppress the increase in blood pressure and reduce the development of vascular, heart, and kidney damage. Many of these studies used germline knockout animals.
In addition, small molecules or neutralizing antibodies that target immune mediators have been used to determine the effect of selective blocking on experimental hypertension.
These drugs target both innate ( eg IL-1, TLR4) and adaptive ( eg IL-17, CD80/86) immune systems. Careful analysis of these studies helps to determine potential therapeutic targets, but also highlights the impact of treatment options and animal model choices on the outcome of BP and target organ damage.
Regarding blood pressure and organ system prognosis, immunomodulatory drugs and animal levels and clinical evidence.
Image source: https://pubmed.ncbi.nlm.nih.gov/34698811/
Although experimental, genetic and clinical evidence to support the immune system involved in inflammation and hypertension and its effects associated blood vessels, kidneys and heart reasonable, but immunomodulation method has not yet been seen to reduce blood pressure and cardiovascular disease treatment options.
In fact, the clinical evidence reviewed in this article shows that immune targeting has a highly heterogeneous effect on blood pressure and cardiovascular events in a wide range of patients mainly suffering from various underlying immune-mediated diseases.
references
E. C. Murray et al. Therapeutic targeting of inflammation in hypertension: from novel mechanisms to translational perspective. Cardiovasc Res 2021 Oct 26;cvab330. doi: 10.1093/cvr/cvab330.
Therapeutic targeting of hypertension and inflammation: from a novel mechanism to a transformational perspective.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



