What is dysfunction of the cancer immune cycle?
- Gut Bacteria Enzymes Offer Hope for ABO Universal Blood Transfusions
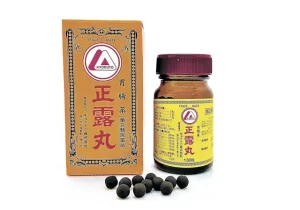
- Well-Known Japanese Medicine Exposed for 30 Years of Data Falsification
- Oregon Reverses Course: From Decriminalization to Recriminalization of Drug Possession
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
What is dysfunction of the cancer immune cycle?
- Was COVID virus leaked from the Chinese WIV lab?
- HIV Cure Research: New Study Links Viral DNA Levels to Spontaneous Control
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
What is dysfunction of the cancer immune cycle?
The use of immune checkpoint inhibitors ( ICIs ) has revolutionized the treatment paradigm for various cancers.
However, despite success in some cancer patients, a significant proportion of patients do not respond to immune checkpoint inhibitors.
A normal cancer immune cycle is a prerequisite for a clinical response to immune checkpoint inhibitors.
Immune checkpoint inhibitors induce meaningful immune responses only when each step of the cycle is activated and functioning properly.
However, activated cancer immune cycles may not be present equally in every patient and cancer type. Ideally, treatment should consider each step of the cancer immune cycle and provide a personalized treatment approach, thus adapting to the dysfunction of the individual patient-specific cancer immune cycle.
Cancer immune cycle
The cancer immune cycle includes several steps to initiate a clinically effective T cell-mediated immune response:
- Tumor cells release antigens
- Antigen uptake by antigen-presenting cells (APCs)
- Transport APCs to regional lymph nodes through the lymphatic system
- Antigen presentation to naive T cells in regional lymph nodes
- Activation of T cells in regional lymph nodes
- T cells travel through the bloodstream to local tumor sites
- T cell-mediated immune response in the tumor microenvironment

All steps of the cancer immune cycle need to function properly in order to generate an effective immune response.
In cancer patients, the cancer immune cycle may be impaired, resulting in barriers to intermediate steps and resulting in deficient anti-tumor immunity, leading to cancer initiation and progression.
Defective tumor antigen release
As the first step in the cancer immune cycle, tumor-specific antigens must be released from dying tumor cells.
Tumor-specific antigens are released after tumor cell necrosis or apoptosis, in addition, antigens must be captured by APCs, mainly dendritic cells ( DCs ), and transported to regional lymph nodes where antigens are presented to naive T cells, thereby priming T cells .
In the absence of dead tumor cells, ineffective antigen release would prevent efficient antigen presentation and further development of the cancer immune cycle, resulting in ineffective recognition of tumor cells by T cells.
Therefore, without the release of antigens from the tumor cells, an immune response in the form of a T cell attack would not arise.
In this way, the complete cancer immune cycle that induces cancer cell death will restart, releasing additional tumor-associated antigens, which will further restart the cancer immune cycle and deepen the tumor-specific T cell response.
The frequently observed correlation between high TMB and ICI response could be explained by the higher availability of tumor neoantigens in the presence of a high mutational burden.
Therefore, the higher the TMB, the higher the response rate to ICI therapy. In addition, the structure of antigens, especially the antigen presentation mechanism, can also affect whether they are taken up by APCs, and human leukocyte antigen ( HLA ) binding capacity can affect this specific process.
Thus, another mode of immune evasion is to split the antigen presentation system through acquired mutations of the HLA component β2 microglobulin or loss of HLA alleles, resulting in restricted antigen presentation and T cell recognition.
Therapeutically, cancer vaccination is a possible strategy to overcome deficiencies in antigen release and presentation and is currently being extensively investigated.
So far, vaccines have shown some clinical benefit in carcinoma in situ or minimal residual disease.
Furthermore, combination chemotherapy and/or radiotherapy may induce tumor antigen availability due to induction of apoptosis/necrosis.
Therefore, combined chemotherapy and ICI therapy is clinically more effective than ICI alone. The implementation of combination chemotherapy, radiotherapy or other vaccination strategies is currently being studied extensively.
In addition, other novel immunomodulatory therapies such as histone deacetylase ( HDAC ) inhibitors, which have been identified to increase the expression of PD-L1, major histocompatibility complex ( MHC ) class I/II molecules, and cancer species line mutations, thereby increasing antigen-based tumor immunogenicity.
HDAC inhibitors have shown clinically meaningful results in hematological malignancies such as B-cell lymphoma and are currently being investigated in combination with ICIs to boost the immune response and may show efficacy in solid tumors.
Impaired T cell priming in regional lymph nodes
Presentation of tumor-specific antigens to naive T cells triggers the priming and activation of effector T cells. Importantly, the distribution of effector T cells and regulatory T cells has a crucial impact on the effectiveness of the immune response.
Since most tumor antigens are derived from self-antigens, tumor-specific antigens may not be adequately recognized as “outside” antigens by APCs or T cells, which would lead to the priming and activation of regulatory T cells rather than effector T cells.
Therefore, this process must be accompanied by immunogenic signals, such as pro-inflammatory cytokines ( such as IL-1, IFN-α, TNF-α ) and co-stimulatory factors ( such as CD27, OX40 ), to promote immunity rather than lead to Tolerance to specific antigens.
In addition, within regional lymph nodes, the matching T cell receptor ( TCR ) for each mature T cell must be activated. If there is no match, that is, due to low TCR sequence diversity, no immune response will be generated.
Furthermore, immune checkpoint blockade has been shown to affect the diversity of the TCR gene repertoire, thereby enhancing antitumor immunity at this specific stage of the cancer immune cycle.
The affinity between tumor antigen-MHC complexes and TCRs also plays an important role in the activation of antitumor activity.
Adoptive T cell therapy is a potential therapeutic approach to overcome insufficient activation of effector T cells by reintroducing genetically modified autologous T cells into patients.
Chimeric antigen receptor ( CAR ) T cells targeting tumor surface antigens have shown significant clinical benefit in hematological malignancies. Similar approaches targeting recombinant antigen-specific TCRs are under investigation.
Bispecific or trispecific T cell engagers ( BiTE, TriTE ) are linkers between endogenous cytotoxic T cells and antigens expressed by cancer cells, and the continuous engagement of cytotoxic T cells and cancer antigens leads to T cell proliferation , enhance T cell-mediated immune response, and increase tumor specificity.
Currently, hundreds of bispecific T cell binders are under clinical investigation in phase I–III clinical trials. In addition, cytokines and co-stimulatory factors involved in T cell priming and activation can also serve as therapeutic targets.
Another important mechanism of immune escape occurring in regional lymph nodes is the control of T cell activation through additional inhibitory immune checkpoints.
The CTLA-4 inhibitory antibody ipilimumab blocks CTLA-4, thereby preventing the interaction of its ligands CD80 and CD86 in regional lymph nodes.
Thus, the negative regulation and inhibition of T cell activation is blocked, leading to the expansion of T cells.
Systemic factors that suppress circulating tumor-specific T cells
Activated effector T cells must reach the local tumor site through the blood circulation. However, factors in the bloodstream may affect the sustainability of activated T cells.
Circulating neutrophils increase due to cancer-mediated myelopoiesis. Neutrophils can suppress T cell-mediated antitumor responses by secreting inhibitors such as arginase, nitric oxide synthase ( NOS ), and phagocytosis-associated oxidase ( PHOX ), which further generate reactive oxygen species ( ROS ) and inhibit T cell activation.
Elevated systemic inflammatory markers, such as neutrophil-to-lymphocyte ratio ( NLR ) and acute-phase protein C-reactive protein ( CRP ), are associated with lower treatment response and overall survival in solid cancers.
Therefore, inhibition of pro-inflammatory cytokines may be a possible way to enhance anti-tumor immune responses. Inhibition of IL-6 has been reported to have a beneficial effect on the efficacy of anti-PD-L1 therapy in preclinical studies, and a phase I-II clinical trial (NCT04191421) of an IL-6 inhibitor in combination with anti-PD-1 therapy is currently underway middle.
In addition, canakinumab, an anti-IL-1β antibody, is undergoing clinical trials in combination with anti-PD-1 therapy in NSCLC patients ( NCT03631199 ).
In conclusion, many targets of systemic inflammatory molecules are under preclinical and clinical investigation and may have applications in immunotherapy in the future.
Immunosuppressive signals in the local tumor microenvironment
In the local tumor microenvironment, the composition of the vascular structure and the cytokine gradient affect the effect of T cell homing, which in turn affects the anti-tumor immune response.
Pathologically composed and activated endothelial cells have been shown to hinder the efficient influx of T cells.
Once in the local tumor microenvironment, tumor-specifically activated T cells face multiple immunosuppressive factors.
Tumor cells themselves or tumor-infiltrating lymphocytes can express immune checkpoints, such as PD-1/PD-L1, LAG-3, TIM3, and TIGIT, to suppress immune responses.
In addition, immunomodulatory molecules released by tumor cells, such as indoleamine 2,3-dioxygenase ( IDO ), as well as cytokines ( i.e., IL-6, IL-10, TGF-β ), can prevent effective T cell action , and even produce intratumoral T cell depletion.
Regulatory T cells, myeloid-derived suppressor cells ( MDSCs ), and tumor-associated macrophages, especially M2-type macrophages, in the tumor microenvironment can increase immune suppression and tumor cell evasion.
Currently, combination therapy has the potential to address the suppression of tumor immune evasion by targeting the immune microenvironment.
Combination chemotherapy has the potential to increase PD-L1 expression on tumor cells, thereby improving the response potential to PD-1 axis ICI therapy.
Furthermore, in addition to chemotherapy, combined inhibition of vascular endothelial growth factor ( VEGF ) with anti-angiogenic drugs such as bevacizumab or VEGF-targeted TKIs may potentially enhance anti-PD- 1 blockers of the anti-tumor immune response are currently under investigation ( NCT03396926, NCT04879368 ).
Targeting Wnt/β-catenin signaling pathway combined with PD-1 targeting ICI is thought to improve T cell priming and T cell infiltration into tumor microenvironment, because Wnt/β-catenin pathway is associated with dendritic cells, tumor-associated macrophages cells as well as regulation of regulatory T cell infiltration, which was tested in early clinical trials ( NCT01351103 ).
In addition, immunosuppressive cytokines can also be specifically targeted, such as against IDO ( NCT03854032, NCT03915405 ), IL-6/IL-6R ( NCT04191421, NCT04691817 ), IL-10 ( NCT03382912, NCT02009449 ) and TGF-β ( NCT04429542 ), as a combination immunotherapy for advanced solid cancers.
Approaches that combine PD-1/PD-L1 inhibitors to inhibit the DNA damage repair ( DDR ) pathway, such as poly ADP-ribose polymerase ( PARP ) inhibitors or circulating protein-dependent kinase 4/6 ( CDK4/6 ) inhibitors are also a way.
Because dysfunctional DDR is thought to play a role in activating the host immune system.
For example, PARP inhibitors can enhance antitumor immunity by activating the STING pathway, thereby increasing the recruitment of chemokines and further inducing cytotoxic T cell function.
In addition, other cell types in the tumor inflammatory microenvironment, such as MDSCs, tumor-associated macrophages, and tumor-associated fibroblasts, can also be targeted for therapy, potentially improving the resulting antitumor immune response.
Summary
All steps of the cancer immune cycle may exhibit impaired function, resulting in ineffective intermediate processes that reduce tumor-specific immune responses.
In fact, immune escape and resistance mechanisms may lead to ineffective ICI blockade therapy.
Therefore, there is a need to specifically address dysfunctions that may occur at several steps in the cancer immune cycle. A personalized biomarker approach can help identify patient-specific disturbances in the immune cycle, allowing for targeted combination therapy.
Currently, many promising novel immunomodulatory therapeutic strategies and their combinations are currently being investigated in the clinic, with the potential to achieve meaningful immune responses in cancer patients.
In conclusion, in the future, a comprehensive understanding of the unique interactions between the patient’s immune system and cancer cells, as well as the specific underlying immune escape mechanisms, is needed to guide the selection of personalized immunotherapy for cancer patients.
references:
1. Immune escape mechanisms and therapeutic approaches in cancer: the cancer-immunity cycle. The Adv Med Oncol. 2022;14: 17588359221096219.
What is dysfunction of the cancer immune cycle?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.