Minimal clinically important difference (MCID): Definiton and Calculation
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
Minimal clinically important difference (MCID): Definiton and Calculation
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- What is the difference between Atorvastatin and Rosuvastatin?
- How long can the patient live after heart stent surgery?
Minimal clinically important difference (MCID): Definiton and Calculation.
Evaluating the efficacy of analgesic intervention usually relies on statistical analysis of research data, but a statistically significant “effective” intervention does not necessarily bring significant clinical benefits.
Therefore, the current pain research field introduces the smallest The concept of minimal clinically important difference (MCID) focuses on the improvement of analgesic interventions perceived by patients, rather than just the statistical difference in pain scores.
This issue brings a review of “Regional Anesthesia & Pain Medicine”, let us deepen our understanding of MCID, an evaluation indicator.
As part of modern multi-modal analgesia strategies, regional analgesia has been proven to reduce pain and reduce the use of opioids. Some systematic reviews and meta-analysis have reported that regional analgesia techniques such as fascial space block or local infiltration block have statistically significant analgesic effects.
However, whether the numerical changes of indicators such as the VAS score or opioid consumption are equivalent to clinical benefits and patients’ perceived improvement is still worthy of further discussion.
This article aims to explain the concept of MCID and its calculation process, carefully evaluate the current process and conclusions of clinical research evaluating the effect of regional analgesia, and predict the development direction and new methods of the field of acute postoperative pain research.
Definition and calculation of MCID
The term MCID was first proposed by Jaeschke in 1989 and was originally applied to the research background of chronic heart and lung diseases.
It is the smallest amount of change in the score of a scale recognized by the patient without considering the side effects and cost.
Simply put, the MCID represents the smallest difference that the patient thinks is important or meaningful to it.
MCID is different from statistically significant differences. Statistically significant differences represent differences from a mathematical point of view, and are not necessarily equivalent to clinically significant differences.
Some interventions with statistical differences may not be significant or not important at all to improve the patient’s symptoms or the quality of rehabilitation.
MCID is especially suitable for large-sample clinical research. In this type of research, it may be found that certain interventions have statistical differences when compared between groups, but the clinical differences are not obvious.
This is why when evaluating the effect of an intervention, statistical significance is a necessary condition, but it is not yet sufficient to fully prove its superiority.
MCID calculation usually adopts “anchor method” and “distribution method”, or the “joint calculation method” which adopts both, and the “Delphi method (expert consensus method)” can also be used as a complement and supplement to the above method.
The anchor method is also called the effectiveness standard method, which is to match the patient self-rating scale (such as VAS or NRS) with a scale that measures changes (ie, “anchor”).
The commonly used “anchor” has the subjective “universal grading Table “(Global assessment rating, GAR), this scale quantifies the improvement, deterioration or no change described by the patient.
However, due to the subjective nature of the GAR scale, it is often necessary to refer to other quantifiable indicators such as the consumption of painkillers to further verify the reliability and effectiveness of the anchor point.
As there is no gold standard anchor point, it is usually recommended to combine multiple independent reference indicators to reflect the reactivity of different individuals.
Figure 1 shows the classic anchoring method. 2 or 3 points represent the smallest clinically significant reduction in pain score, that is, the MCID value, which can be understood as a minimum decrease of 2-3 points in the VAS score after a certain analgesic intervention. At this time, the patient can feel that the pain improves.
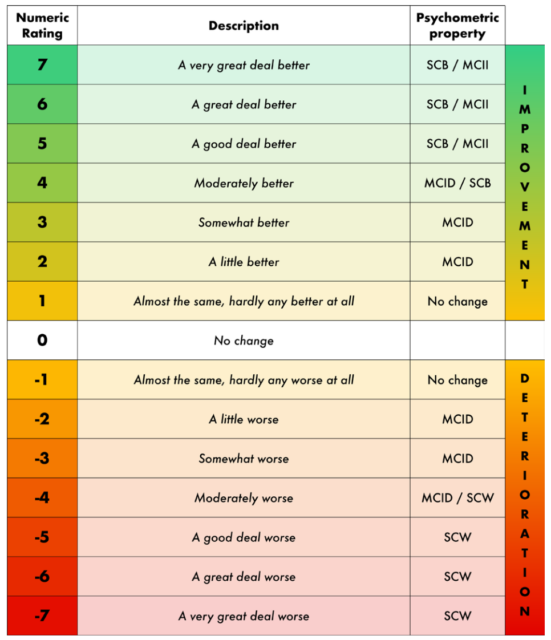 Figure 1. The GAR scale calculates MCID for anchors
Figure 1. The GAR scale calculates MCID for anchors
The distribution method is based on the statistical distribution description index of the patient self-rating scale to calculate the MCID value.
Commonly used distribution indexes include standard error (SEM), standard deviation (SD), effect size (ES), and minimum detectable change (minimum detectable change). , MDC).
Generally 0.5 SEM or 1 SD represents 1 MCID value. The distribution method cannot explain the smallest change in clinical significance, because it lacks an anchor to connect with the subjective feelings of the research object. Therefore, the validity of the distribution method is still controversial.
There are often some changes that are statistically significant and patients or clinicians believe that it is not necessarily clinically meaningful.
In the joint calculation method, the above two complementary methods are used to calculate the MCID value, for example, the distribution method is used to calculate 0.5 SD, SEM, etc., and the anchor method is used to determine the minimum clinical change.
When these factors are fitted together, an MCID value that is not limited by methodology is obtained, which can more accurately reflect clinically significant group-level changes.
Regardless of the calculation method used, an accurate understanding of the meaning of MCID is the most important.
It provides a quantifiable tool to evaluate and compare the clinical impact of interventions perceived by patients and clinicians, and ultimately to guide clinical decision-making.
In addition, MCID can also be applied to assess the quality of restoration.
Limitations of MCID
There are many limitations in the MCID determination process.
For example, even for the same patient, using different measurement methods will result in different MCID values, so comprehensive consideration is required.
The patient’s current pain score may be adjusted based on the expected value rather than the initial baseline level.
Other restrictions, such as misunderstanding of the meaning of “improvement” and recall bias, may have an impact on MCID.
Even for the same pain background, the MCID value is not a constant, it will change with the level of pain before treatment.
In other words, the higher the pain score reported by the patient, the higher the MCID value, because a greater degree of pain relief is required after treatment to achieve a satisfactory state.
In addition, as MCID says literally, it represents the “minimal” rather than the “ideal” clinical change.
Therefore, it does not indicate the success of the clinical treatment, but only the smallest change that the patient is satisfied with.
At present, the validity and reliability of MCID in the field of postoperative acute pain have not been fully confirmed, and it needs to be verified by more reliable research data in the future.
All in all, due to the inherent limitations of the MCID concept and its calculation process, other concepts and methods need to be supplemented to evaluate the effectiveness of analgesic intervention more comprehensively.
Calculate the MCID of acute postoperative pain based on chronic/non-surgical pain data
Due to the lack of specific acute postoperative pain background data, it has become the norm to calculate MCID values based on data from other different patient groups.
A meta-analysis by Hussain et al. pointed out that thoracic nerve block is an effective analgesic method for breast cancer surgery.
Compared with systemic analgesia, the VAS score of each postoperative period has a MCID value of 1.1, and 24 hours of opioid use The amount is reduced by 27mg (oral morphine equivalent), and then this MCID value is calculated based on chronic breast cancer pain data rather than acute postoperative pain.
A meta-analysis by Abdallah et al. evaluated the effect of a single intramuscular groove block for shoulder surgery analgesia.
They concluded that the intermuscular groove block cannot reduce the resting VAS score and the 8h postoperative period.
The 12-hour opioid consumption has a MCID value of 0.9-1.1. This value is derived from the data of emergency trauma patients and other non-surgical populations.
As the MCID of acute postoperative pain of breast cancer and shoulder joint surgery has not been reported, the reliability of the MCID value calculated from chronic or non-surgical pain is also unknown.
Previous studies on various types of chronic pain have shown that the MCID value varies greatly. For example, the MCID value for scleroderma is 0.8, while the MCID value for trigeminal neuralgia is 8.2 (see Figure 2).
There are few studies on MCID for acute postoperative pain, and only some studies are difficult to apply to the current research standards due to various factors, such as the inclusion of different patient groups, surgical methods, analgesic methods, and mixing of existing therapies Or interfering factors such as different baseline pain values.
In addition, previous studies have mostly focused on moderate to severe pain, and there are few data on mild pain. To this day, we do not know whether the MCID of acute pain is pain intensity-specific, surgical procedure-specific, or both.
MCID and response to treatment vary with population characteristics and research background. Therefore, the MCID values of different surgeries or patients are not the same, which is not the same as the conclusion drawn under the background of chronic pain.
In addition, for patients with chronic pain, the MCID value of postoperative pain relief may be different from that of patients without this condition.
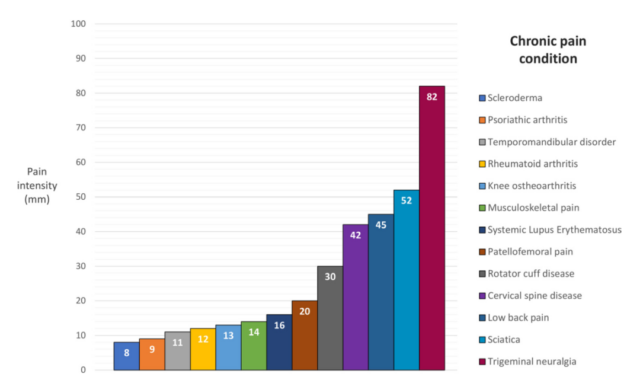
Figure 2. Different types of chronic pain have different MCIDs
MCID and opioid consumption
Currently, the relationship between opioid savings and clinically significant analgesic interventions is not clear. Intuitive judgments that can reduce opioid consumption or opioid-related mid- to long-term side effects, or improve functional recovery, can be regarded as clinically important or meaningful interventions.
However, while many studies have pointed out that regional analgesia can reduce opioid consumption, few have mentioned that it can reduce opioid-related adverse reactions.
This raises the question, how much milligram reduction in opioid consumption can be considered a clinically significant and meaningful improvement?
In addition, in addition to the inability to control pain, the patient’s additional demand for pain medication is also affected by other factors.
For example, only when the patient feels that the pain relief effect exceeds the potential side effects (such as nausea and vomiting), a request for supplementary opioids will be made. Obviously, patients will weigh the pain relief and reduce adverse reactions. Based on this, the amount of opioid savings cannot effectively evaluate the effect of analgesic treatment.
MCII, SCB and PASS
The ideal effect of pain treatment should be that the patient feels well and not just feels slightly improved (the latter is MCID). Tubach et al. put forward another important concept—minimal clinical important improvement (MCII), which is the smallest change in the patient’s perception of symptom improvement.
This improvement enables the patient to reach a state that can accept the current symptoms, namely PASS (patient acceptable symptom state) means that the patient currently feels satisfied (MCII value> 4) rather than just feeling slightly better (MCID> 2 or 3).
Substantial clinical benefit (SCB) is also a measure of psychological latitude, which measures the amount of change that patients perceive substantial or significant improvement, which is equivalent to MCII in a sense. The calculation of SCB can apply the calculation method of MCID. Martin et al.
In a retrospective study on chronic hip pain, based on the anchoring method and the distribution method, the MCID value of the VAS scale was calculated to be 1.5, and the SCB value was 2.27. That is to say, the VAS score decreased by at least 1.5 to be felt. To change, drop 2.27 to reach PASS (patient acceptable state).
PASS represents the pain score that the patient is satisfied with the current symptoms. It can be expressed in the upper quartile of the VAS score of all patients who feel satisfied, or in short, the pain score when 75% of the patients feel satisfied .
Unlike MCID, MCII, and SCB, the PASS value of acute pain is a constant. Taking the 10-point VAS scale as an example, it is generally a constant between 3 and 4 points. Because PASS is an “all-or-nothing” constant threshold, it is not affected by the baseline value, and has been verified in chronic pain, so it can be used for acute postoperative pain related research.
All in all, MCID can be understood as the smallest change in score for feeling clinical improvement, MCII and SCB are the score changes for achieving ideal clinical improvement, and PASS is the score change for achieving a relatively more satisfactory state.
Figure 3 visually shows the relationship between the concepts of MCID, MCII, SCB and PASS. The columns A and B in the figure represent two types of pain with different baseline levels.
The ordinate represents the 10-point VAS scale. The height of the column represents the initial pain score (baseline value), the length of the dark yellow area is the MCID value, the length of the dark yellow + light yellow area is the MCII/SCB value, the height of the blue area is the pain score after treatment, and the height of the red dashed line is the PASS value.
Take the A column as an example, the baseline VAS of pain is 8 points; the MCID value is 1, that is, the VAS is reduced by at least 1 point. Patients can feel pain relief; the MCII/SCB value is 5 (> 4), that is, the VAS is reduced by 5 points.
The patient can feel substantial clinical benefit or improvement; the PASS value is 3.3, that is, when the VAS drops to 3.3 points, the patient can be satisfied with the current state.
It can be seen from the figure that MCID is a subset of MCII/SCB, and PASS is a constant threshold, which is approximately equal to the difference between the baseline value and MCII/SCB.
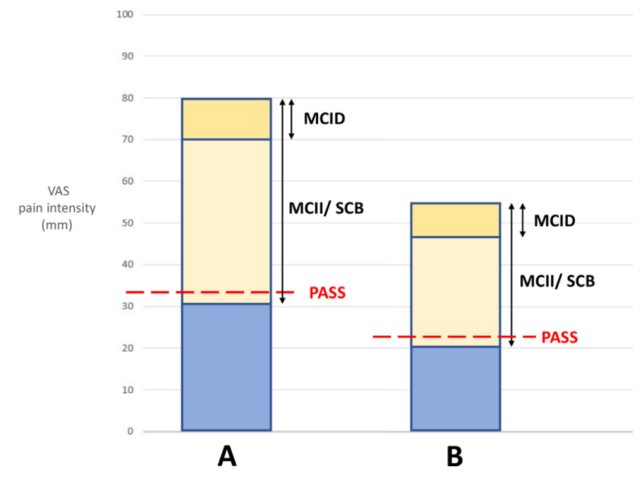
Figure 3. The relationship between MCID, MCII, SCB, PASS
Future research direction
In perioperative pain research, we should pay more attention to clinical improvement than statistical differences.
After using a certain analgesic intervention, it is the key that patients feel pain relief or achieve a satisfactory state, rather than being stuck.
Because of the statistical difference in the changes in VAS or opioid consumption, the “statistical difference theory” can be discontinued.
When using indicators such as VAS or opioid consumption, attention should also be paid to other factors that may affect patient relief or satisfaction, such as adverse reactions, rehabilitation quality, gastrointestinal function recovery, mobility and sleep quality.
The GAR score and the VAS score should be used organically instead of using the latter in isolation. The proportion of patients who achieve MCII, SCB or PASS is an ideal indicator for evaluating postoperative pain management strategies.
However, since these indicators are mostly derived from chronic pain research, in the future, we should pay attention to the research in the background of perioperative acute pain and postoperative recovery, and further determine the MCID value of different operations and different populations.
If data from chronic pain background have to be used to calculate the MCID of acute postoperative pain, the calculation method and relevant research background should also be clearly clarified, such as the types of chronic pain, population characteristics, and baseline pain levels.
It is helpful to clarify these data. To calculate the sample size and effect size more accurately in future clinical controlled studies or meta-analysis can also avoid the possibility of drawing wrong research conclusions due to the inherent limitations of MCID.
Believe that if we can make good use of the MCID and other emerging methods and indicators, it will provide a more accurate basis for evaluating the efficacy of perioperative analgesia measures, and will also benefit patients’ relief and recovery.
Expert Comments:
In previous clinical studies, indicators such as VAS, NRS score, or opioid consumption were often used to evaluate the analgesic effect.
Sometimes these indicators have significant statistical differences, but they do not have any significance for the patient’s own pain perception. It is the key that the patient feels pain relief or achieves a satisfactory state.
In this issue of Bone Anesthesia Journey, we reviewed MCID. In recent years, some high-scoring articles in the field of anesthesia and pain have also adopted this method.
The biggest feature of MCID is to highlight clinical differences. To do truly meaningful clinical research, not only pay attention to statistical differences, but also pay attention to the degree of benefit from a clinical perspective.
Even if the study results are statistically different, but the patient’s benefit or improvement is not obvious, it still does not meet the requirements of MCID.
Of course, there is still no gold standard for the formulation of MCID, and all calculation methods also have certain shortcomings and limitations, and they need to be used in a reasonable combination.
Secondly, many of the existing values are also based on chronic pain research, which has limited significance for acute pain and perioperative pain.
This is also the direction that needs to be paid attention to and intensively cultivated in the future.
Minimal clinically important difference (MCID): Definiton and Calculation
(source:internet, reference only)
Disclaimer of medicaltrend.org



