Intraoperative blood pressure monitoring in obese patients-arterial catheter
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Intraoperative blood pressure monitoring in obese patients-arterial catheter, finger cuff method and oscillometric method
Intraoperative blood pressure monitoring in obese patients-arterial catheter. The proportion of obese patients in lumbar spine and joint surgery is relatively high.
The best blood pressure monitoring method for obese patients is still unclear. Although there are many invasive and non-invasive monitoring methods, there is little understanding of the consistency of different methods.
This period brings a study of “Anesthesiology” to compare three methods including the new fingering method, let us learn together.
Research Background
Obesity patients have a high risk of cardiac complications during surgery, and close monitoring of blood pressure is essential for such patients. However, choosing the best perioperative blood pressure monitoring method for obese patients is a major challenge in clinical practice.
Continuous invasive blood pressure monitoring using arterial catheters (ie, intra-arterial blood pressure monitoring) is the clinical gold standard, but there is a risk of potential complications, such as permanent ischemic injury (average incidence rate of 0.1%), bleeding (0.5%), or local infection (0.7%).
In addition, for severely obese patients, the placement of the arterial catheter itself presents technical challenges. The oscillometric method uses an inflatable cuff for non-invasive blood pressure monitoring, but it can only provide intermittent data, and the measurement accuracy is affected by the appropriate cuff size and cuff position.
Ideally, the cuff size needs to match the circumference of the limb (usually the upper arm) selected by the oscillometric method to obtain a reliable value. Obese patients have an increased circumference, and the upper arms are usually conical rather than cylindrical. Therefore, it has been proposed that for obese patients, the forearm can be used instead of the upper arm for oscillometric pressure measurement.
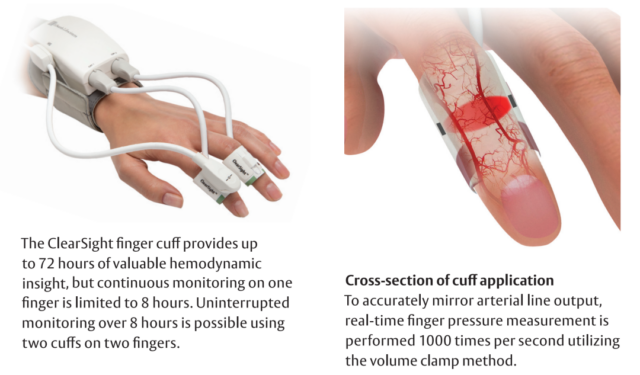
In view of the limitations of continuous intra-arterial pressure measurement and intermittent non-invasive oscillometric pressure measurement, a new technology that can achieve continuous non-invasive blood pressure monitoring is expected to become a new choice for obese patients during surgery. One of the continuous non-invasive blood pressure monitoring technologies is the finger cuff-based vascular unloading technology, also known as the volume clamp method.
As a prerequisite for routine blood pressure monitoring, the finger cuff method needs to be researched to clarify its comparability with established reference methods, including continuous intra-arterial pressure measurement using arterial catheters and intermittent non-invasive blood pressure monitoring using oscillometric methods. This study aims to test the hypothesis that the finger cuff method is more consistent with the intra-arterial pressure measurement than the oscillometric method.
Research method
This prospective study used Bland-Altman analysis, four-quadrant graphs, consistency analysis (assessing the ability of manometric methods to change with blood pressure), and error grid analysis (description of the clinical relevance of measurement differences) to analyze 90 patients who underwent bariatric surgery For obese patients, compare the consistency of intra-arterial pressure measurement (gold standard), finger cuff method and oscillometric method (upper arm, forearm, and calf).
1. Research design and subjects
Inclusion criteria: Elective laparoscopic bariatric surgery with body mass index (BMI) ≥40kg/m2 (gastric bypass, sleeve gastrectomy, and gastric banding surgery) adult patients, American Society of Anesthesiologists (ASA) physical status classification <IV level. Exclusion criteria: presence of edema around the upper or lower extremities, vascular or anatomical abnormalities, history of ipsilateral axillary or inguinal lymph node resection, carpal tunnel syndrome, modified Allen test negative and no obvious ipsilateral ulnar artery pulsation, atrial fibrillation. The data was collected from September 2011 to February 2013.
2. Anesthesia
According to the judgment of the anesthesia team, all patients received similar general anesthesia treatment. The representative combination of general anesthesia induction and endotracheal intubation is: propofol (1~2mg/kg adjusted body weight [adjusted body weight, ABW]) + fentanyl (1μg/kg ABW) + lidocaine 100 mg + Luo Curonium (0.8mg/kg ABW) or succinylcholine (1.5mg/kg ABW), intravenously. Sevoflurane/desflurane is used in combination with fentanyl and hydromorphone for the maintenance of general anesthesia. During preparations for abdominal surgery and when the skin is sutured, the patient is in a horizontal lying position, and the patient is in the reverse Trendelenburg position during the operation. Both arms are extended abducted and fixed on padded arm plates.
3. Blood pressure measurement
The author performed continuous intra-arterial pressure measurement through radial artery catheterization (reference method), continuous non-invasive finger cuff pressure measurement (test method), and intermittent non-invasive oscillometric pressure measurement on the upper arm, forearm, and calf.
Continuous arterial pressure measurement: After general anesthesia is induced, a 20G arterial catheter is inserted into the patient’s radial artery and connected to a disposable pressure sensor. During the entire test, the pressure sensor is at the same level as the right atrium. Check the damping characteristics of the transducer through a quick flush test and correct abnormal damping if necessary.
In order to continuously record the non-invasive finger cuff blood pressure, the author uses the ccNexfin finger cuff system (BMEYE B.V., Holland), now known as ClearSight (acquired by Edwards Lifesciences, USA). The ccNexfin/ClearSight system uses an inflatable finger cuff to measure the arterial blood flow of the finger through an infrared plethysmograph. Based on the automatic feedback system, the finger cuff is inflated and deflated to keep the blood flow constant throughout the heart cycle and indirectly based on the required finger cuff pressure. Rebuild the blood pressure waveform. According to the manufacturer’s instructions on the appropriate size, choose to place the finger sleeve on the middle phalanx of a suitable middle finger or ring finger. The cardiac reference system is responsible for compensating for the hydrostatic pressure difference between the heart level and the finger cuff level, and is placed at the right atrium level during the entire test.
Intermittent non-invasive oscillometric pressure measurement uses conventional adult upper arm, forearm and calf cuffs to measure pressure at the corresponding parts. If the blood pressure measurement value can be obtained, the cuff is considered to be suitable. If the cuff fails to wrap around the limb or fall off automatically when inflated, it means that the cuff at the limb has failed. No tape or other tools are used to save the attempt to measure. The calf oscillometric pressure measurement performed while the patient was in the reverse Trendelenburg position was not included in the analysis because the hydrostatic pressure difference would affect the difference between the calf pressure measurement and the intra-arterial pressure measurement.
Intra-arterial, finger cuff method, upper arm and forearm pressure measurements are all performed on the patient’s ipsilateral limb to avoid the possible influence of the blood pressure difference between the bilateral limbs on the test results. The cuff for calf pressure is located on the right leg. The results of intra-arterial and oscillometric pressure measurement are displayed on the patient monitor (Philips MP90 monitor). The finger cuff pressure measurement results are displayed on the dedicated monitor for the ccNexfin system.
During the entire trial, the authors recorded the mean arterial pressure, systolic blood pressure, and diastolic blood pressure at 6 different time points. Each measurement cycle starts with simultaneous intra-arterial and finger cuff pressure, followed by forearm and upper arm pressure measurement, and finally calf pressure measurement. The 6 time points were: 15 minutes before the pneumoperitoneum in the horizontal lying position, 3, 15, 30, and 45 minutes after the 30° reverse Trendelenburg position pneumoperitoneum, and 3 minutes after the exhaust in the horizontal lying position. Visually inspect the intra-arterial pressure waveform before each inspection point to correct any observable artifacts or abnormalities in the blood pressure waveform.
4. Statistical analysis
Patient characteristics are expressed as mean±standard deviation or percentage of absolute number, and blood pressure values are expressed as mean±standard deviation and interval. Calculating the Pearson correlation coefficient represents the distribution of the measurement values of the finger cuff method and the upper arm, forearm, and calf manometry, and its relationship with the intra-arterial pressure measurement.
Repeated measurement data Bland-Altman analysis was used to evaluate the consistency between finger cuff method and upper arm, forearm, calf pressure measurement and intra-arterial pressure measurement, and calculate the mean, standard deviation and 95% consistency limit of the difference (bias) (The mean of the difference ± 1.96 × standard deviation). The relationship between the mean and the difference is shown in the Bland-Altman diagram, and the results are tested by linear regression analysis. Using the four-quadrant diagram, the 5mmHg area was excluded, and the coincidence rate was calculated to describe the trend consistency of the finger cuff method and the upper arm, forearm, and calf oscillometric pressure measurement compared with the intra-arterial pressure measurement.
Continuous error grid analysis is used to classify the differences between blood pressure monitoring methods according to clinical importance. The error grid is a scatter plot, the X axis is the reference value of blood pressure measurement, and the Y axis is the blood pressure measurement value of the corresponding detection method. It contains a total of 5 risk areas. Each pair of blood pressure measurements is classified into one of 5 risk areas. The risk area represents the patient risk caused by different treatment interventions that may be caused by measurement differences.
It is divided into: Area A, no risk; Area B, low risk; Area C, medium risk; Area D, high risk; Area E, critical risk . The boundary of the risk area was investigated by 25 experts. Based on the experience and judgment of the experts, five blood pressure ranges that may require the following treatment measures are defined: hypotension requiring urgent treatment; hypotension with appropriate treatment; no intervention required; hypertension with appropriate treatment ; High blood pressure that needs urgent treatment. Because measurement differences can cause patient risks, experts classify the risk according to the combination of “the blood pressure measurement value of the detection method used is in the range of i” and “the reference blood pressure measurement value is in the range of j”.
Experts summarized and weighted answers to the 5 risk levels to get the error grid risk area. In order to better describe the different risk areas of the error grid, the color map is used for the map, and the color of the risk free to the critical risk changes from green to red. The patient risk caused by measurement differences can be visually assessed through a color-coded continuous error grid, and can be quantitatively analyzed by calculating the absolute and relative numbers of the paired measurement values in the risk area.
Research results and conclusions
A total of 108 patients were recruited in the study due to difficulty in inserting arterial catheters (n=11), technical failure of blood pressure monitoring equipment during operation (n=3), surgical changes (n=1), patients withdrew from participation (n=1), It was found that the neglected exclusion criteria (n=1) and case cancellation (n=1) excluded a total of 18 patients. The final analysis of the data of 90 patients showed that the mean ± standard deviation of BMI was 48 ± 7 kg/m2. Table 1 summarizes the patient characteristics. Cuff measurement failed in 8 cases of upper arm, 1 case of forearm and 11 cases of calf blood pressure. In some cases, there was no suitable upper arm (6 cases) or calf (24 cases) cuffs, and no such situation occurred in the forearm pressure measurement.
Table 1. Patient characteristics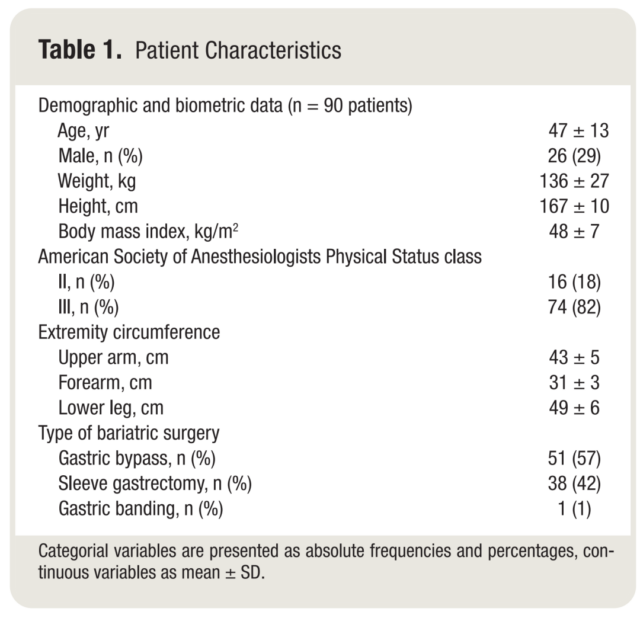
Bland-Altman analysis showed that the mean difference in mean arterial pressure between finger cuff method and intra-arterial pressure measurement (± standard deviation, 95% agreement limit) was -1mmHg (±11mmHg, -23 to 21mmHg), and systolic blood pressure was -7mmHg (±14mmHg, -35 to 20mmHg), diastolic blood pressure is 0mmHg (±11mmHg, -22 to 22mmHg) (Figure 1A, Table 2). The Bland-Altman analysis of upper arm, forearm, and calf pressure measurement compared with intra-arterial pressure measurement is shown in Figure 1B-D, Table 2. Compared with the difference between the mean arterial pressure and diastolic blood pressure measured by the finger cuff method and the intra-arterial measurement, the mean and standard deviation of the difference of the oscillometric method (three measurement positions) are larger.
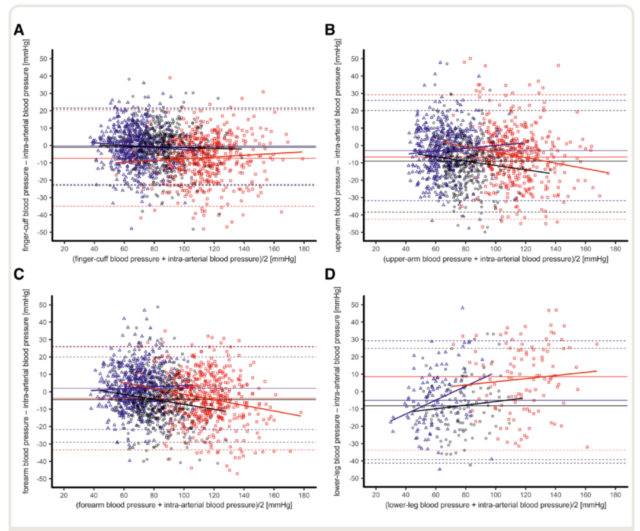
Figure 1. Bland-Altmant diagram, showing the pressure measurement results of radial artery catheter intra-arterial pressure measurement and finger cuff technology (A), upper arm oscillography (B), forearm oscillography (C) and calf oscillography (D) Consistency.
Table 2. Comparison of non-invasive (finger cuff and oscillometric method) and intra-arterial (radial artery catheter) pressure measurement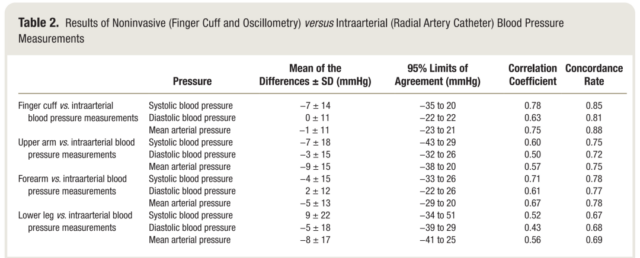
The four-quadrant graph analysis showed that the blood pressure changes consistent with the intra-arterial pressure measurement by the finger cuff method were as follows: mean arterial pressure 88%, systolic blood pressure 85%, and diastolic blood pressure 81% (Figure 2; Table 2). The four-quadrant diagram analysis of the comparison between the pressure measurement of the upper arm and the forearm and the intra-arterial pressure is shown in Table 2. For the mean arterial pressure, the coincidence rate of blood pressure changes between the oscillometric method (three parts) and the intra-arterial pressure is lower than that of the finger cuff method.
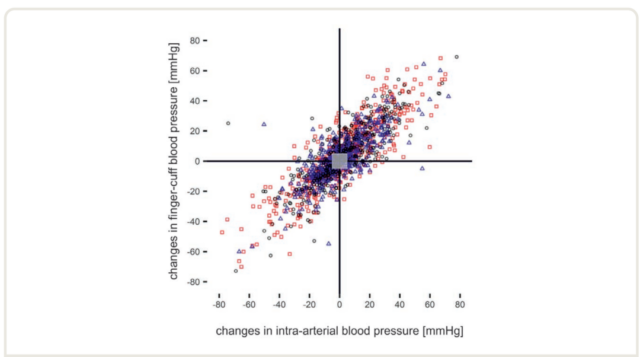
Figure 2. The 5mmHg area excluded in the middle of the four-quadrant graph shows the consistency of the trend of changes in the results of radial artery catheter intra-arterial pressure measurement and finger cuff technique pressure measurement over time.
Error grid analysis compared the results of finger cuff method and intra-arterial pressure measurement and found that the ratios of the average arterial pressure paired measurement values in the risk A to E area were 77.1%, 21.6%, 0.9%, 0.4%, and 0.0%, which were located in risk A. The ratio of paired systolic blood pressure to the E area was 89.5%, 9.8%, 0.2%, 0.4%, and 0.2% (Figure 3A and B; Table 3).
Table 3. Error grid analysis results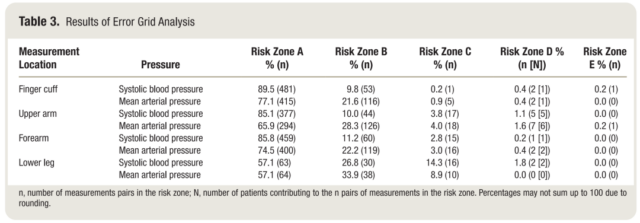
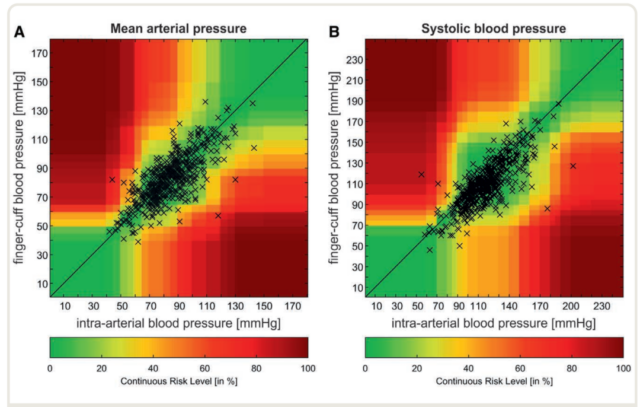
Figure 3. Error grid analysis compares the difference between the mean arterial pressure (A) and systolic pressure (B) obtained by the intra-arterial pressure measurement of the radial artery catheter and the finger cuff technique.
The above results show that the mean arterial pressure and diastolic blood pressure obtained by the intra-operative finger cuff method in obese patients are more consistent with the intra-arterial pressure measurement than the oscillometric method. The forearm oscillometric method is superior to the upper arm and calf oscillometric method.
Discusion:
This study is a comparative study of methods. In a wide range of blood pressure values, it compares the application of intra-arterial pressure measurement with finger cuff method and upper arm, forearm, and calf pressure measurement in obesity patients during bariatric surgery. The absolute consistency and trend consistency between finger cuff pressure measurement and intra-arterial pressure measurement were only moderately consistent. However, the error grid analysis shows that 99% of the finger pressure measurement values are located in the risk A (no risk) and B (low risk) areas. For mean arterial pressure and diastolic blood pressure, the absolute consistency and trend consistency of finger cuff method and intra-arterial pressure measurement are better than oscillometric method (all three parts). From the perspective of absolute consistency and trend consistency with intra-arterial pressure measurement, forearm blood pressure monitoring is better than upper arm and calf pressure measurement.
Unlike previous studies that only compared finger cuff method with intra-arterial pressure measurement, this study also compared the difference between oscillometric method and intra-arterial pressure measurement. The upper arm, forearm, and calf pressure measurement is less consistent with the intra-arterial pressure measurement. However, the error grid analysis results of this study show that, compared with the intra-arterial pressure measurements, more than 90% of the average arterial pressure paired values are located in no-risk or low-risk areas.
An important new finding of this study is that the absolute consistency and trend consistency of the forearm pressure measurement and the intra-arterial pressure measurement are better than the upper arm pressure measurement. This finding of intraoperative patients is consistent with the postoperative results of obese patients in previous studies, and supports the choice of forearm oscillometric pressure measurement for this type of population. Although these results further support that forearm oscillometric pressure measurement can be used as a routine alternative to upper arm pressure measurement, the authors believe that further prospective studies are needed to compare the forearm before deciding which part of the oscillometric pressure measurement can be used as a routine recommendation for obese patients. The rationality of the upper arm oscillometric method for obesity surgery patients.
In this study, compared with the oscillometric method (all three parts), the mean arterial pressure and diastolic blood pressure obtained by the finger cuff method are smaller and more consistent with the intra-arterial pressure value. Therefore, from the perspective of absolute consistency and trend consistency with intra-arterial pressure measurement, the performance of finger cuff technology to measure mean arterial pressure and diastolic blood pressure is better than that of oscillometric method. In addition, unlike the intermittent pressure measurement of the oscillometric method, finger cuff technology can provide continuous blood pressure monitoring. Therefore, for obese patients who require invasive procedures such as anesthesia or sedation, finger cuff technology may be a reasonable alternative to intermittent non-invasive oscillometric manometry. There are no studies to explore the relationship between such findings and the prognosis of severely obese patients.
The choice of perioperative blood pressure monitoring method should also consider the cost. Medical systems in different countries and even different medical systems in the same country differ greatly in the cost, maintenance, and training costs of various blood pressure monitoring equipment. Arterial catheter placement requires training of medical personnel. Compared with non-invasive blood pressure monitoring such as finger cuff method or oscillometric method, this technique is also more time-consuming. At present, the material cost of finger cuff technology is also higher than that of arterial catheter set or oscillometric method. This study did not focus on the cost-benefit analysis of different blood pressure monitoring technologies. In addition to discussing which method should be selected for perioperative blood pressure monitoring in the future, the impact of personnel costs and material costs of different methods on postoperative complications should be compared.
The patients in this study represent a typical bariatric surgery population, not a population of obese patients with a wide range of ages. The latter corresponds to more extensive surgical procedures and may have advanced cardiovascular complications. This relatively selective research population may limit the generalization of the results of this study. The author used the ipsilateral arm to measure the pressure of all upper limbs in order to avoid the mixed influence of bilateral blood pressure differences. Whether the arterial catheter can block the blood flow of the arm and affect the measurement of finger cuff blood pressure is not discussed in this study.
In short, for the measurement of mean arterial pressure and diastolic blood pressure in obese patients, the consistency of finger cuff method and intra-arterial pressure measurement is better than that of oscillometric method. For such patients, the forearm oscillometric method is better than the upper arm or calf oscillometric method.
Expert Comments:
Blood pressure monitoring is one of the most important intraoperative monitoring, and the change of its value provides a basis for intraoperative anesthesia management. Accurate acquisition of blood pressure changes is essential for maintaining the blood supply of important organs during surgery.
There are mainly two commonly used monitoring methods: non-invasive blood pressure monitoring by oscillometric method through an inflatable cuff or invasive blood pressure monitoring by inserting a catheter into an artery. The non-invasive method is intermittent monitoring and the accuracy of measurement is low; the invasive method is accurate but has many complications and the operation is more difficult.
Non-invasive continuous blood pressure monitoring between the two seems to be a better choice. There have been many products available, and the comparative study with invasive blood pressure measurement has always been a hot spot in clinical research.
In this study, the ClearSight system was used, and the finger cuff method was used to measure continuous non-invasive blood pressure.

The study analyzed 90 obese patients undergoing bariatric surgery, and compared the accuracy and consistency of finger cuff method, multi-site oscillometric method and invasive continuous pressure measurement at different points in the operation. The study found that the mean arterial pressure and diastolic pressure obtained by the finger cuff method were more consistent with the intra-arterial pressure measurement than the oscillometric method, but the systolic blood pressure data did not reflect the difference. The forearm oscillometric method is superior to the upper arm and calf oscillometric method.
In the current clinical anesthesia work, such a situation often occurs. The anesthesiologist not only wants to observe the patient’s continuous blood pressure changes, but also worry about the risks that may be brought about by invasive methods. Between risks and benefits, anesthesiologists face a dilemma. For example, blood pressure fluctuations during general anesthesia induction, sudden hemodynamic fluctuations during smooth operation, and equipment failures that often occur in cuff pressure measurement are all good indications for non-invasive continuous pressure measurement.
The results of this study on obese patients are encouraging, but further large-sample studies are needed to compare ordinary patients. If the cost can be reduced, this technology is expected to replace the oscillometric method as a method of routine blood pressure monitoring, thereby improving clinical safety.
(source:internet, reference only)
Disclaimer of medicaltrend.org



