ARNI: ACC updates the expert consensus on heart failure treatment
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
ARNI: ACC updates the expert consensus on heart failure treatment
ARNI: ACC updates the expert consensus on heart failure treatment. On January 11, 2021, the American College of Cardiology (ACC) updated the expert consensus on the treatment of patients with heart failure with reduced ejection fraction (HFrEF), and published the detailed content in the “JACC” magazine.
On January 11, 2021, the American College of Cardiology (ACC) updated the expert consensus on the treatment of patients with heart failure with reduced ejection fraction (HFrEF), and published the detailed content in the “JACC” magazine.
The following mainly describes the drug treatment (GDMT) section of the guideline:
1. For patients with HFrEF who have newly progressed to stage C, the renin-angiotensin system inhibitor ARNI/ACEI/ARB or β-blockers should be used for treatment. In some cases, both types of drugs can be used at the same time. Regardless of the order in which the drugs are used, the two types of drugs should be adjusted to the maximum tolerated dose or target dose in time.
2. When the patient has clinical manifestations of congestion (warm, damp, cold), the renin-angiotensin system inhibitor ARNI/ACEI/ARB is better tolerated; there is no congestion (warm, dry, cold) ), β-blockers are better tolerated. For patients with decompensated clinical manifestations, β-blockers are not recommended.
3. For HFrEF patients, only β-blockers recommended by the guidelines and supported by evidence-based evidence, including bisoprolol, carvedilol, and metoprolol succinate, can be used, with specific starting and target doses See the table below:
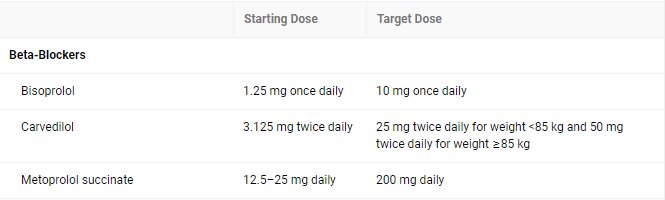
4. For patients without heart failure decompensation and higher dose contraindications, the β-blocker dose should be adjusted every 2 weeks; for frail patients or patients with abnormal hemodynamics, longer adjustment intervals are required . For non-hypotensive patients with stable clinical conditions, rapid titration may be more reasonable.
After the dosage is adjusted, the patient should be informed that the condition of heart failure may deteriorate temporarily, and the specific clinical manifestations may include dyspnea, fatigue, erectile dysfunction, and dizziness.
5. When the patient does not have hypotension, electrolyte imbalance, renal metabolic disorder, ACEI/ARB-related angioedema, ARNI is the first choice for renin-angiotensin inhibitors, and the dose can be adjusted once every two weeks. If ARNI cannot be used, ACEI/ARB should be used (without contraindications).
A clinical study published in the top medical journal “NEJM” in 2019 found that sacubitril and valsartan (ARNI) is significantly better than enalapril in the treatment of patients with heart failure with reduced ejection fraction There is no significant difference in safety:
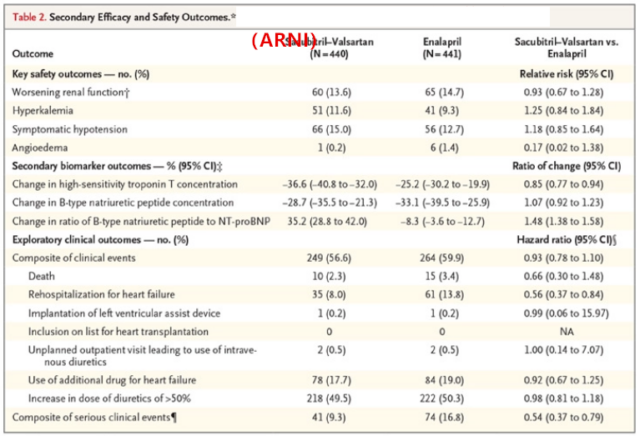
When titrating ARNI/ACEI/ARB, care should be taken to monitor the patient’s renal function, blood potassium and blood pressure. In order to achieve the best ARNI/ACEI/ARB titration treatment plan, diuretics can be used appropriately.
6. For patients with chronic HFrEF receiving β-blockers and ARNI/ACEI/ARB, aldosterone antagonists should be considered (no need to wait until other drugs reach the target dose), during which attention should be paid to monitor renal function and serum potassium.
7. In the absence of contraindications, the combined addition of SGLT2 inhibitors (such as dapagliflozin, which has been tested and verified) is more beneficial to patients, especially for patients with New York Heart Function Class III to IV. During treatment Need to pay attention to monitor the patient’s weight and related clinical symptoms.
8. For patients who have used the target dose or the maximum tolerated dose of β-blockers, and the heart rate is still greater than 70 beats per minute, an additional 2 weeks of adjuvant ivabradine can be used to reduce the heart rate.
9. Abnormal renal function and hyperkalemia are common symptoms during GDMT treatment. During the first 1-2 weeks of ARNI/ACEI/ARB or increased dose, attention should be paid to monitoring and evaluating renal function and blood potassium.
For patients with hyperkalemia, low-potassium diet should be instructed, and FDA-approved potassium-lowering drugs sodium zirconium cyclosilicate and patiromer can be used. Patients with diagnosed kidney disease need to pay attention: for patients with moderate renal insufficiency, if the starting dose of sacubitril and valsartan (ARNI) has been determined, no adjustment is required; for patients with severe renal insufficiency, the starting dose Should be reduced to 24/26 mg twice a day. Despite the lack of definitive evidence, ACEI/ARB is generally considered safe for patients with severe renal insufficiency. When the patient is accompanied by severe renal insufficiency or serum potassium >5.0 mEq/L, aldosterone antagonists are forbidden.
10. When patients with chronic HFrEF start receiving GDMT treatment, it is usually recommended to have regular assessments every 3-6 months. According to the needs of the condition, some patients need shorter reassessment intervals.
11. It is recommended to use echocardiographic strain imaging to assess the heart condition of patients with heart failure. When the patient’s condition changes, the priority is to use echocardiography. If echocardiography is not a good assessment of left ventricular ejection fraction, it is recommended to use radionuclide ventriculography or MRI.
12. For patients with heart failure whose left ventricular ejection fraction recovers to more than 40%, when there is no clear cause (such as tachycardia cardiomyopathy) that can cause the left ventricular ejection fraction to drop, GDMT should be continued.
13. It is recommended to check BNP and NT-proBNP to evaluate the severity and prognosis of patients with heart failure. However, the use of ARNI drugs will reduce the degradation of BNP, while NT-proBNP is not affected.
14. For patients receiving GDMT, if they have high-risk characteristics or poor treatment effects, they should be referred to a heart failure specialist. High-risk characteristics include one or more of the following factors:
① Need to use inotropic drugs intravenously;
② NYHA III-IV with severe fatigue or hyperemia;
③ Systolic blood pressure ≤90mm Hg or symptomatic hypotension;
④ Creatinine ≥1.8mg/dL, or BUN≥43mg/dL;
⑤ Atrial fibrillation, ventricular arrhythmia, ICD repeated electric shock;
⑥ In the past 12 months, have two or more emergency visits or hospitalizations due to worsening heart failure;
⑦ Cannot tolerate the optimal dose of β-blockers and/or ACEI/ARB/ARNI and/or aldosterone antagonists;
⑧ Deterioration of the disease, such as increased edema, increased biomarkers (BNP, NT-proBNP, etc.), worsening of exercise test results, hemodynamic decompensation or imaging remodeling performance;
⑨ Use validated risk models to further evaluate and get high mortality risk results, such as the Seattle heart failure model.
15. Regularly assess the patient’s adherence to medication. In order to improve patient compliance, pay attention to the following: strengthen patient education during and before discharge; stand on the patient’s standpoint and consider the patient’s ideas; use simple and understandable language; try to simplify medication Plan; strengthen multidisciplinary interaction; use mobile medical procedures and tools to remind and record patient data, etc.
References:
1. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. Jan 11, 2021.
(source:chinanet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



