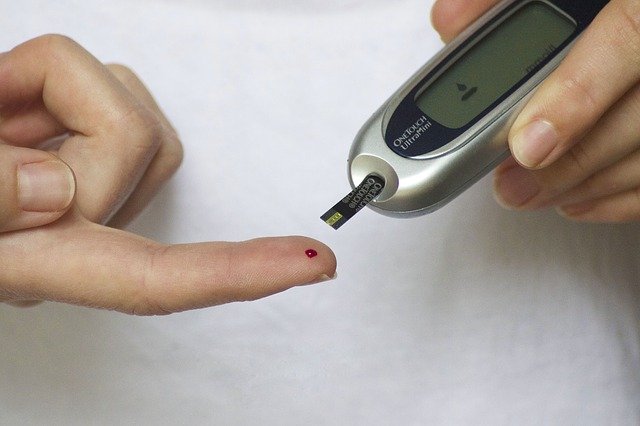
How to interpret the blood routine of diabetic patients?
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
How to interpret the blood routine of diabetic patients?
How to interpret the blood routine of diabetic patients? Blood routine is the most basic clinical examination and one of the auxiliary examinations commonly used in clinical practice.
In recent years, studies have found that related parameters in blood routine are independent risk factors and predictors of the occurrence and development of diabetes and its complications, which have become a research hotspot.
01. White blood cell parameters
1. Increased white blood cell count (WBC)
Studies have shown that inflammation plays an important role in the pathophysiology of T2DM and its complications.
As an inflammatory marker, white blood cell count mediates the body’s inflammatory response. A survey showed that in addition to blood pressure, body mass index (BMI), total cholesterol (TC), blood triglycerides (TG), and LDL-C in type 2 diabetic patients, WBC was significantly higher than that of non-diabetic patients.
Another study observed 116 patients with diabetes mellitus with increased white blood cells. The enrolled patients were only given symptomatic treatments such as hypoglycemic and ketone reduction. The blood white blood cell count and neutrophil percentage of all enrolled patients were significantly lower on the third day of treatment. On the first day, it was confirmed that there is no direct correlation between the increase of white blood cell in type 2 diabetic patients and the infection, and the increase of peripheral blood white blood cell count may also occur in diabetic patients without infection.
Studies have shown that the risk of diabetes increases with the increase in white blood cell count, which is positively correlated with insulin resistance, islet function, atherosclerosis, glucose and lipid metabolism, and blood sugar levels; in addition, a number of studies on diabetes complications suggest that Patients with diabetic microangiopathy also have elevated white blood cell counts.
Increased white blood cell count is an important factor in diabetic retinopathy, nephropathy, and peripheral neuropathy. Chinese scholars believe that T2DM patients with WBC ≥ 5.23 × 10⁹ should be screened for peripheral neuropathy.
Remarks:
In view of the fact that the white blood cell count of diabetic patients can be increased without infection, therefore, the white blood cell count alone as the basis for diabetes co-infection has certain limitations.
For diabetic patients with increased white blood cell count and suspected of infection, other inflammatory indicators should be combined when necessary, combined with comprehensive judgments such as clinical manifestations and signs.
2. Neutrophils (NE), lymphocytes (LC), monocytes (MC)
The survey showed that in T2DM patients, NE, MC and activity were significantly increased, while LC was significantly lower than that of non-diabetic patients. Previous studies have pointed out that monocytes, lymphocytes, and neutrophils are involved in the inflammatory process of diabetic atherosclerosis. Lymphopenia is a common sign of chronic inflammation, and low lymphocyte count is clearly related to coronary artery disease and myocardial infarction.
In addition, recent studies have also found that NE and MC are also elevated in patients with diabetic retinopathy and diabetic nephropathy, suggesting that it is not only related to diabetic macrovascular complications, but also related to diabetic microvascular complications.
Remarks:
Because WBC, NE, LC, MC, etc. are susceptible to drugs, autoimmune diseases, tumors, infections, trauma and other stress factors, a single indicator is not enough to objectively evaluate the body’s oxidative stress and inflammation.
In recent years, studies have found that blood-derived indicators such as neutrophil/lymphocyte ratio (NLR) and lymphocyte/monocyte ratio (LMR) can stably reflect the body’s inflammatory state.
02. Red blood cell parameters
1. Red blood cell count (RBC)
The RBC of diabetic patients binds to endothelial cells through the cxcl16/sr-pso signaling cascade, and the RBC exposed to phosphatidylserine will increase the coagulation cascade, accelerate thrombosis, and further aggravate the microvascular disease in diabetic patients.
Studies have suggested that the decrease in RBC count may be closely related to the occurrence of diabetic microvascular complications. Studies have also found that treating anemia in diabetic patients or correcting the decrease in the number of RBCs can slow down the development of diabetic microvascular disease, especially diabetic patients with anemia should be treated in time to reduce the occurrence of diabetic microvascular complications.
2. Red blood cell distribution width (RDW)
Red blood cell distribution width (RDW) is an indicator for evaluating the variability of red blood cell volume and is mainly used for the differential diagnosis of anemia. In recent years, RDW has become a research hotspot. Studies at home and abroad have found that RDW is a risk factor for coronary heart disease, heart failure and kidney disease. RDW reflects high levels of oxidative stress and chronic inflammation, and is a new prognostic marker for diabetic patients.
In diabetic patients, increased RDW can increase the risk of diabetes complicated by macrovascular and microvascular disease. A study observed 809 cases of T2DM patients, and found that the risk of diabetes complications increased with the increase of RDW, and the higher the RDW, the worse the prognosis.
In the study of RDW level and diabetes complicated with coronary heart disease, it was found that 13.25% is an effective node to determine whether a patient has coronary heart disease, with a specificity of 0.771 and a sensitivity of 0.629. The study also found that elevated RDW is a high risk factor for DKD, and elevated RDW is significantly associated with decreased glomerular filtration rate, decreased albumin and hemoglobin, and other more serious glomerular damage.
3. Mean Red Blood Cell Volume (MCV)
Studies have shown that the MCV of DM patients is significantly higher than that of non-DM patients.
Increased blood sugar leads to damage to the activity of certain enzymes on the red blood cell membrane, changes in the osmotic pressure of the cell membrane crystals, and the tissue fluid enters the cells, thereby increasing the volume of RBC; in addition, long-term hyperglycemia also changes the function and structure of the cell membrane, and the permeability The change occurs, causing the MCV to rise.
The increase of MCV will obstruct the passage of RBC in the capillaries, and require greater perfusion pressure to overcome the resistance of capillaries, resulting in a further increase in blood vessel wall pressure, stasis of blood flow, thickening of the vessel wall, and further aggravation of circulatory obstacles. Accelerate the progression of DM vascular disease.
03. Platelet parameters
In the current study, the relationship between PLT count and diabetes course and complications is not consistent. Some studies believe that PLT count is elevated in patients with diabetic nephropathy, while some studies deny this result.
Mean platelet volume (MPV), platelet distribution width (PDW) and platelet specific product (PCT) are conventional platelet parameters, which are closely related to the size, shape and structure of PLT. Platelet parameters can reflect the activation state of PLT.
Studies by STEIROPOULOS et al. have shown that the increase of MPV and PDW is positively correlated with the activation of PLT, that is, the higher the MPV and PDW, the higher the activation degree of PLT, and the stronger the functions of PLT such as aggregation, adhesion, and release, so that it has a higher Thrombosis potential.
1. Mean platelet volume (MPV)
Mean platelet volume (MPV) is an important indicator for evaluating platelet function and activity, and is related to the increase in the incidence of cardiovascular and cerebrovascular diseases.
A meta-analysis suggests that MPV has a higher level in DM patients and is closely related to diabetic microangiopathy. MPV value can increase with the progression of diabetic nephropathy (DN) staging. MPV can be used to determine DN staging and monitor DN progress.
2. Platelet distribution width (PDW)
PDW is a specific marker of PLT activation, and the up-regulation of PDW in peripheral blood indicates platelet activation. Compared with non-diabetic people, the PDW of diabetic patients is significantly higher, and PDW is also related to diabetic complications.
04. Blood routine derived indicators
Platelet/lymphocyte ratio (PLR), neutrophil/lymphocyte ratio (NLR) and lymphocyte/monocyte ratio (LMR), etc., have been considered as new inflammatory indicators in recent years, which are in contrast to classic inflammatory mediators (such as CRP). , IL6 and TNFα), etc. are related, but compared with CRP, IL6, TNFα and other inflammatory mediators, its advantages are that it is easier to obtain, does not increase the cost of additional examinations for patients, and has higher stability.
1. Absolute Neutrophil Value/Absolute Lymphocyte Value (NLR)
The research on the relationship between NLR and insulin resistance, diabetes and its complications has been a research hotspot in recent years. Studies have shown that for every 1 unit increase in NLR, the risk of insulin resistance (IR) increases by 7.231 times. A high NLR value may be a reliable predictor of IR. In addition, impaired pancreatic β-cell function, fasting blood glucose levels, and poor blood glucose control are all closely related to high NLR.
It has been reported that for every unit increase in NLR, the risk of diabetic nephropathy increases by 2.088 times. NLR is an independent risk factor for diabetic peripheral neuropathy (DPN) and can be used to predict the occurrence and development of DPN. In addition, the increase of NLR is closely related to diabetic cardiovascular disease and is a risk factor for diabetic cardiovascular disease. NLR ≥ 5.0 is of great significance in predicting re-myocardial infarction and related death.
2. Platelet/lymphocyte ratio (PLR)
Similar to NLR, PLR is also an emerging marker. It is currently believed that PLR can be used as a marker of coronary atherosclerosis, and the ratio is significantly related to the severity of coronary artery disease. However, the relationship between PLR levels and diabetes is still controversial.
Some studies believe that in diabetic patients, a significant increase in PLR can independently predict the 90-day readmission and death risk of high-risk diabetic ketoacidosis patients. In addition, PLR has higher sensitivity and specificity in diagnosing diabetic nephropathy (DN). The sensitivity and specificity of predicting the risk of microalbuminuria in T2DM patients are 71.1% and 68.0%, respectively, which are powerful for DN patients Independent predictor.
However, some studies have shown that PLR exhibits a curve trend of first decline and then rise during the development of diabetes. That is, the PLR level is the lowest in patients with impaired glucose tolerance, the highest in diabetic patients, and the PLR level in patients with new-onset type 2 diabetes is in the middle. PLR may be involved in the development of impaired glucose tolerance.
3. Monocyte/lymphocyte ratio (MLR)
As a new indicator of inflammation, MLR is currently believed to be associated with diabetic retinopathy and diabetic coronary heart disease.
05. Summary
As a routine examination, blood routine is simple, easy to test, universal and ready-to-use. With the deepening of research on various parameters in blood routine, we have found that it helps predict and identify the risk of diabetes and its macrovascular disease, microvascular disease, and then provide clinical diagnosis, evaluation of treatment effects, and prognosis evaluation. Reference.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



