Luminal A Breast Cancer Patients May Not Require Radiotherapy After Breast-Conserving Surgery
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Luminal A Breast Cancer Patients May Not Require Radiotherapy After Breast-Conserving Surgery
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
NEJM: Luminal A Breast Cancer Patients May Not Require Radiotherapy After Breast-Conserving Surgery.
Combining postoperative radiotherapy with breast-conserving surgery has been the standard treatment for early-stage breast cancer patients. However, radiotherapy is time-consuming, costly, and comes with significant short-term and long-term side effects that can seriously affect the quality of life.
In recent years, with the detection of smaller breast cancers, advancements in surgical techniques, and the application of systemic adjuvant therapies, the risk of local recurrence after breast-conserving surgery for breast cancer has significantly decreased.
To improve the quality of life for patients further, researchers have conducted extensive studies to identify low-risk populations and assess the feasibility of exempting them from postoperative radiotherapy.
Recently, The New England Journal of Medicine (NEJM, IF: 158.5) published the results of the LUMINA study, which confirmed that women with Luminal A breast cancer aged ≥55 years, tumor size ≤2 cm, no lymph node involvement, and histological grade 1 or 2, can safely omit postoperative radiotherapy after breast-conserving surgery and receive only endocrine therapy, with a 5-year local recurrence rate of only 2.3%.
Study Design:
This study was a single-arm, prospective, multicenter study involving patients from 26 research centers. Inclusion criteria were women aged ≥55 years, diagnosed with ductal carcinoma, tubular carcinoma, or mucinous carcinoma of the breast, who had undergone breast-conserving surgery, had a maximum tumor diameter of ≤2 cm, clear surgical margins (≥1 mm), negative axillary lymph nodes, and immunohistochemical positivity for ER (≥1%), PR (>20%), and HER2 negativity.
Patients meeting these criteria underwent Ki-67 testing, and those with Ki-67 ≤13.25% were included in the study as Luminal A subtype. All enrolled patients received aromatase inhibitors (anastrozole, letrozole, or exemestane) or tamoxifen as endocrine therapy for at least 5 years but did not undergo breast radiotherapy.
The primary endpoint of the study was ipsilateral breast local recurrence, including true recurrences within ±2 cm of the primary site and margin recurrences, as well as ectopic recurrences in the same breast. Secondary endpoints included contralateral breast cancer, any recurrence (ipsilateral breast, regional lymph nodes, or distant sites), disease-free survival (time from enrollment to any recurrence, contralateral breast cancer, second primary non-breast cancer, or death), and overall survival.
The study’s statistical hypothesis was that if the upper limit of the 90% confidence interval for the 5-year cumulative incidence of ipsilateral breast cancer recurrence was lower than 5%, it would meet the criteria for omitting radiotherapy.
Study Results:
From August 2013 to July 2017, a total of 740 patients were registered, and after Ki-67 testing, 505 patients with Ki-67 index ≤13.25% (Luminal A subtype) were included, with 500 patients included in the intention-to-treat analysis. The baseline characteristics of the patients are shown in the table below. The median follow-up time was 5 years.
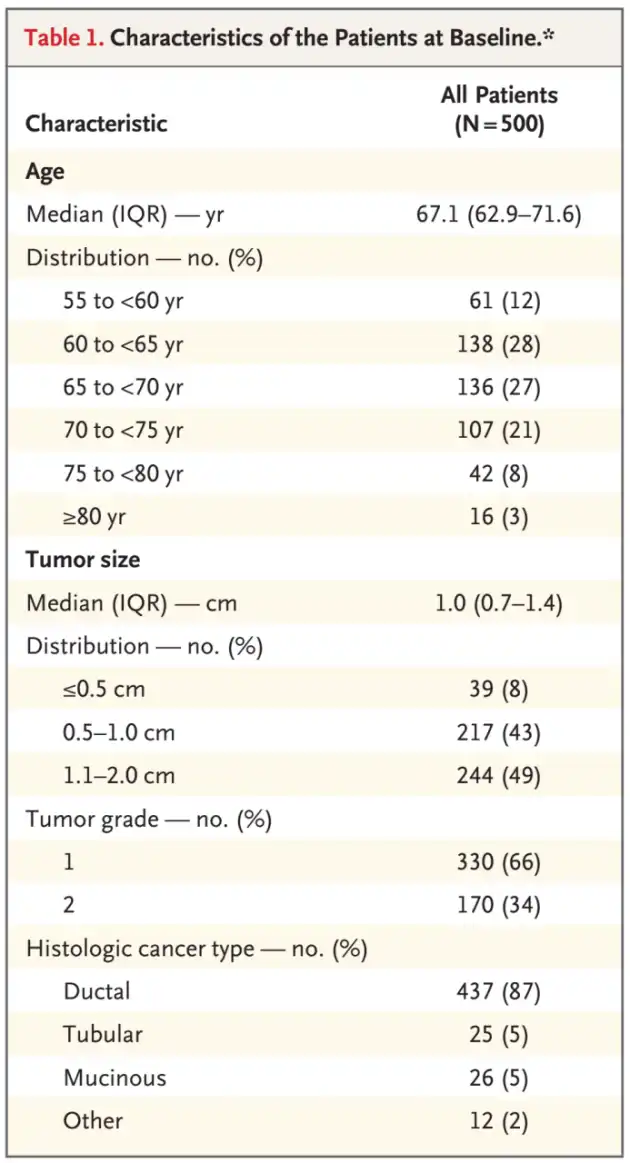
Baseline Patient Characteristics,source: NEJM
Regarding the primary endpoint, at a median follow-up time of 5 years, 10 patients experienced local recurrence. The 5-year cumulative incidence was 2.3% (90% confidence interval [CI], 1.3-3.8; 95% CI, 1.2-4.1), with the upper limit of the confidence interval lower than the predefined 5% boundary. Of the 10 local recurrences, all were invasive, 6 were true recurrences or margin recurrences, and 4 occurred in other areas of the same breast. Sensitivity analysis assuming a 5-year local recurrence rate of the exit patients equal to the upper limit of the 90% confidence interval of the observed patients resulted in an additional 1 patient experiencing local recurrence. Thus, the 5-year local recurrence rate was 2.5% (90% CI, 1.5-4.0), with the upper limit of the confidence interval still below the predefined 5% boundary.
Regarding secondary endpoints, researchers observed 8 cases of contralateral breast cancer, all invasive, with a 5-year cumulative incidence of 1.9% (90% CI, 1.1-3.2). There were 12 cases of any recurrence, including 10 local recurrences, 0 regional recurrences, and 2 distant recurrences, with a 5-year cumulative incidence of 2.7% (90% CI, 1.6-4.1).
In terms of disease-free survival, there were 11 recurrences, 7 cases of contralateral breast cancer, 23 cases of second primary cancers, and 6 deaths reported as the first event, totaling 47 events. The 5-year disease-free survival rate was 89.9% (90% CI, 87.5-92.2). During the follow-up period, there were a total of 13 deaths, with only 1 related to cancer. The 5-year overall survival rate was 97.2% (90% CI, 95.9-98.4).
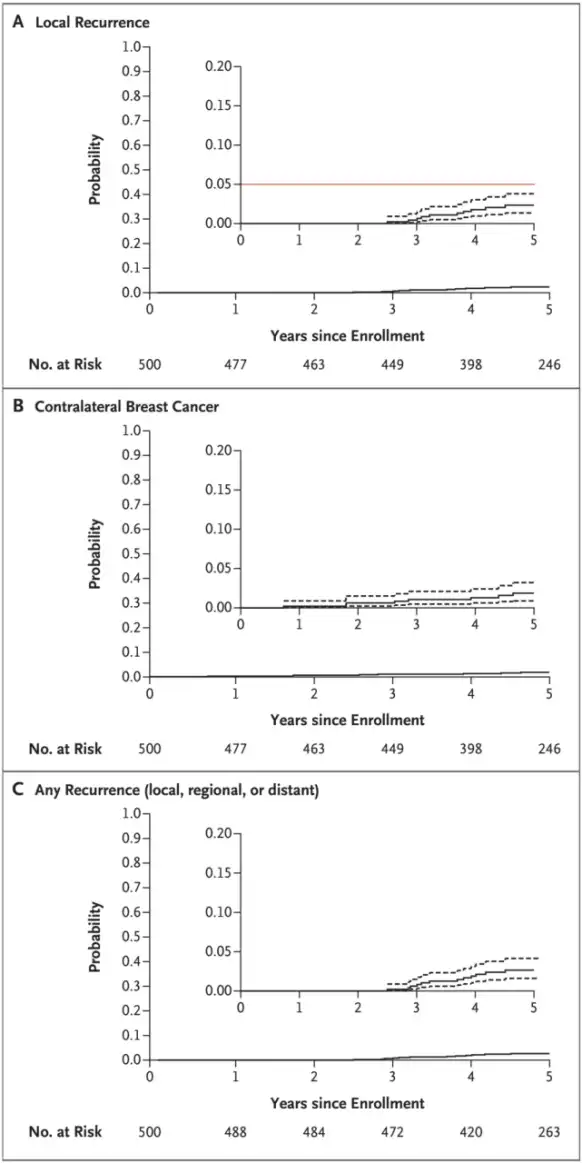
Cumulative incidence of ipsilateral local recurrence (A), contralateral breast cancer (B), and any recurrence (C). Source: NEJM
Discussion:
Prior research has shown that postoperative radiotherapy can reduce the risk of ipsilateral breast cancer recurrence. However, many patients with a low risk of local recurrence can be cured with surgery and endocrine therapy alone. Therefore, the goal for patients at extremely low risk of local recurrence is to improve care by omitting radiotherapy and thus avoiding its short-term and long-term side effects.
Researchers had previously found that using immunohistochemical analysis for intrinsic subtype analysis could independently predict the risk of local recurrence. They further assessed whether combining clinical-pathological factors with intrinsic subtype analysis could identify a group of patients at low enough risk to omit radiation therapy. The results showed that patients with Luminal A subtype who were at low clinical risk (age >60 years, T1N0, grade 1 or 2) had the lowest risk of local recurrence (1.3%) after breast-conserving surgery alone.
As a result, researchers conducted this multicenter prospective study to validate that combining molecular biomarkers with clinical-pathological factors can identify patients who can safely omit radiotherapy. The study showed that in Luminal A breast cancer women aged ≥55 years, T1N0, grade 1 or 2, omitting radiotherapy after breast-conserving surgery and receiving only endocrine therapy resulted in a very low 5-year local recurrence rate. The upper limits of the observed recurrence rates’ 90% confidence intervals and 95% confidence intervals met the predefined boundaries, further confirming that these patients are candidates for omitting radiotherapy.
Compared to genomic analysis, the immunohistochemical markers used in this study, such as Ki67, ER, PR, and HER2, are cost-effective, reproducible in multiple central laboratories, and more suitable for clinical application. However, this study was a single-arm study with a follow-up time of only 5 years. It is necessary to conduct multicenter large-sample randomized controlled trials with extended follow-up times to clarify long-term prognosis and late recurrence risk, enhance the reliability of the research results, and select the best personalized treatment plan for breast cancer patients.
Reference:
Whelan TJ, Smith S, Parpia S, et al. Omitting Radiotherapy after Breast-Conserving Surgery in Luminal A Breast Cancer. N Engl J Med. 2023;389(7):612-619. doi:10.1056/NEJMoa2302344
NEJM: Luminal A Breast Cancer Patients May Not Require Radiotherapy After Breast-Conserving Surgery.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



