Arthroscopic synovectomy: Difficulties and Countermeasures
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
Arthroscopic synovectomy: Difficulties and Countermeasures
Arthroscopic synovectomy: Difficulties and Countermeasures. Partial synovectomy can be done through the anterior internal approach and the anterior external approach. The total synovectomy includes the resection of 20% of the posterior joint cavity and must be completed with 6 approaches.
(1) Posture
The patient generally adopts the supine position. When the patient is in the supine position, the lower extremity of the surgical side can be slightly abducted, the knee joint can be placed naturally on the side of the operating bed, and the lower limb of the opposite side can be placed flat on the operating table, with a tourniquet and routine disinfection drapes. And add a one-time waterproof sheet. Connected to the arthroscopic lavage system, the lavage fluid is generally 3000ml of saline plus 1ml of 0.1% epinephrine, which can better maintain a clear vision during the operation.
(2) Approach selection
1. Anterolateral approach (Figure 10-1)
The conventional knee flexion is 90°, located at the junction of 1cm on the lateral knee joint line and 1cm on the lateral edge of the patellar tendon, that is, the lateral knee and eye. Insert a round head puncture cone and cannula into the incision, and enter the joint cavity through the subcutaneous tissue, subpatellar fat pad and joint capsule. This entrance is located above the lateral joint line and about 1cm below the patella. If the entrance is too close to the joint line, the lateral half The anterior angle of the plate may be torn or damaged, or it may penetrate into the joint cavity from below the lateral meniscus when the arthroscope is inserted. If the entrance position is too high, the arthroscopy will enter the space between the femur and tibial condyle, which will affect the observation of the posterior angle of the meniscus and other posterior structures. If the arthroscopy is inserted close to the edge of the patellar tendon, the arthroscopy can penetrate the fat pad, affecting the field of view, and making operation difficult.

Figure 10-1 Anterior medial and anterolateral approach of knee arthroscopy
2. Anteromedial approach (Figure 10-1)
The entrance position is similar to the anterolateral approach, located at the junction of 1 cm on the medial knee joint line and 1 cm of the medial edge of the patellar tendon, that is, the medial knee and eye. The above two entrances are the most commonly used entrances. The conventional positioning method is to quote the method of foreign authors. 1cm beside the patellar tendon may be too large. In our country, 0.5cm beside the patellar tendon is appropriate. In addition, it should be based on the patient’s age, body shape, and body fat. Factors such as thinness and thickness should be considered for positioning. The author’s experience is that at the medial and lateral knees and eyes, the incision site should be at the most depressed area of the anterior patellar tendon of the knee joint before the fluid is filled in the joint cavity. After the fluid is filled with the joint cavity, the incision site should be the fullest.
3. Anterior median approach
Between the anterior, medial and lateral entrances, it is located at the center of the patellar tendon 1cm below the tip of the patellar tendon. If there is an abnormal increase in the Q angle, knee valgus, etc., it should be appropriately inward; the entrance height should be adjusted appropriately when encountering high or low patella , As far as possible into the condyle level, the entrance slightly higher or lower will affect the operation. There is no obvious injury to the patellar tendon through this mouth operation, but the entrance and exit must pass through the fat pad, and the knee pain may occur after the operation.
4. Lateral approach
The outer edge of the quadriceps tendon located 2.5cm above the upper outer corner of the patella. Using the upper edge of the patella as a mark, push the patella outward to find out the patellofemoral joint space, and place the index finger on the upper edge of the patella, approximately at the junction of a transverse finger on the upper edge of the patella and the joint space of the patella. The entrance is The most common approach for placing arthroscopic perfusion tubes.
5. Posteromedial approach (Figure 10-2)
The entrance is located behind the medial collateral ligament, 1cm on the posterior medial joint line, and 1cm behind the posterior medial condyle of the femur, that is, the small triangle area between the posterior and inner edges of the medial condyle of the femur. The knee can be touched at 90°. When using this approach, care should be taken to prevent popliteal vascular nerve injury. The knee joint should not be filled when positioning, and the knee should be bent 90°. The knee joint should be filled during puncture, and the blunt cannula core should be inserted from the upward oblique to the inward direction. If the entrance is to be used during the operation, a long needle can be used for puncture after positioning. If there is fluid outflow to indicate that the needle has entered the joint, the cored cannula can be inserted along the puncture needle position and the direction of travel. The structure of the inner chamber.

Figure 10-2 Schematic diagram of the posterior medial approach of the knee arthroscopy
①Front inside; ②Front outside; ③Middle; ④Inside up; ⑤Outside up; ⑥Outside; ⑦Inside; ⑧Inside; ⑨Outside;
6. Posterolateral approach
Bend the knee at 90°, the intersection point between the upward extension line of the posterior edge of the fibular head and the posterior edge of the femoral shaft, that is, the lower edge of the iliotibial band, the upper edge of the biceps femoris tendon and the posterior outer edge of the lateral femoral condyle, and the posterior outer edge 2cm above the joint. When entering directly from the entrance, the skin incision should be positioned under the condition of the joint cavity not being filled, and then the core sleeve should be inserted after filling the joint cavity, moving inward and downward toward the posterior condyle to touch the surface and then moving inward into the joint cavity. The operation of puncture and placement of the cannula is the same as that of the posterior medial entrance operation to prevent popliteal blood vessel and nerve damage. The entrance is mostly used for inspection and surgery of the structure in the posterior joint cavity.
(3) Resection method
Partial synovectomy can be done through the anterior internal approach and the anterior external approach. The total synovectomy includes the resection of 20% of the posterior joint cavity and must be completed with 6 approaches. Before synovectomy, first conduct a detailed exploration of the joint cavity, starting from the suprapatellar capsule, through the internal and external recesses, tibiofemoral joint, around the medial and lateral meniscus, around the cruciate ligament, and finally observe the posterior joint cavity. Following the above sequence for synovectomy can avoid omissions and make the vision of the joint cavity clearer (Figure 10-3, Figure 10-4).
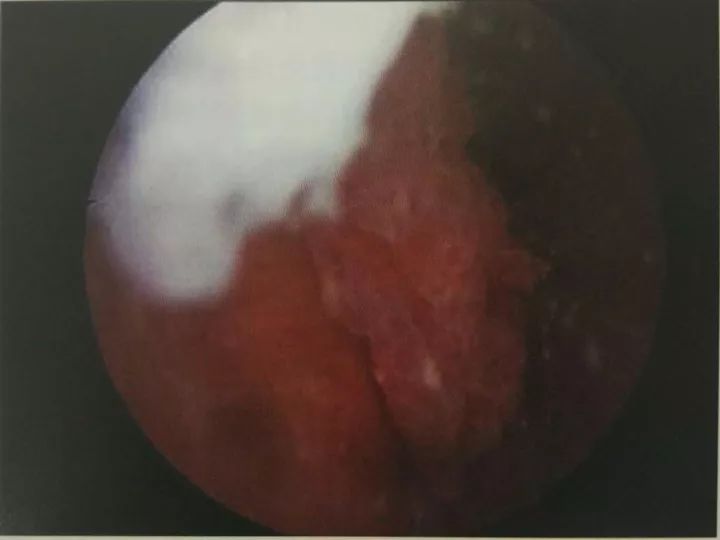
Figure 10-3 Rheumatoid arthritis (view under the microscope)
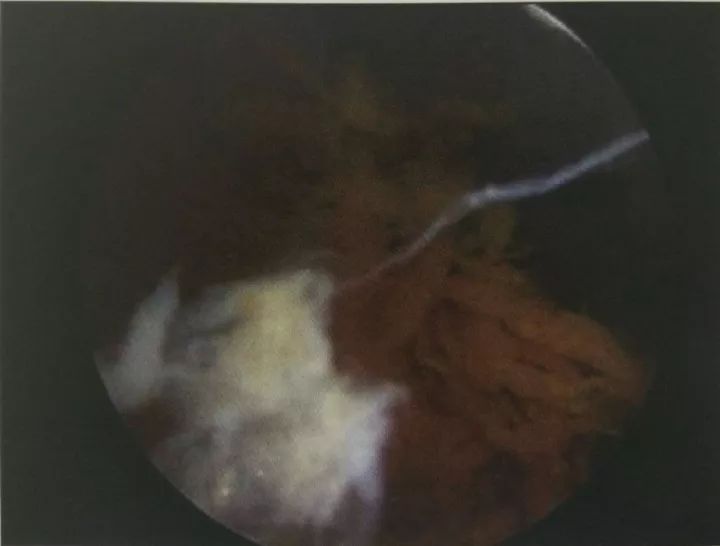
Figure 10-4 Pigmented villous nodular synovitis (view under microscope)
The first step is to observe through the anterior lateral approach. The synovial membrane of the distal end of the suprapatellar sac and the medial recess is resected through the superior external approach or the anterior internal approach. The lateral recess can be viewed from the front and the outside due to the higher external femoral condyle. Observation and surgery are performed using the upper and outer approaches. The synovial membrane at the proximal end of the suprapatellar capsule is farther from the anterolateral approach. The upper lateral approach can be used for observation and anterior and lateral approach.
The second step is to remove the synovial membrane of the tibiofemoral joint cavity. The conventional anterior internal approach and anterior external approach can complete this step, including the intercondylar fossa, the edge and underside of the meniscus, the synovium on the surface of the fat pad, and a small part of the synovial membrane of the posterior joint cavity. If the meniscus is eroded, For trimming or resection, the posterior part of the meniscus has a better view when the knee joint is close to extension. Observation and surgery should be performed in this position. The synovium below the meniscus and the junction of the cartilage synovium can be removed with a curved planer. For the synovial membrane at the outer and posterior edges of the meniscus, the planer can be inserted from the front, inner and outer sides, and the popliteal sac can also be removed. membrane.
The third step is to remove the synovial membrane of the posterior joint cavity. After the intercondylar fossa is cleaned, go through the 70° lens from the front and the inside, enter the posterior and outer joint cavity through the lateral side of the anterior cruciate ligament, the medial side of the femoral lateral condyle, and the posterior corner of the lateral meniscus. The synovial membrane of the joint cavity; on the contrary, through the anterior and external lens, the posterior internal joint cavity is entered through the posterior corner of the posterior cruciate ligament, the lateral femoral condyle, and the medial meniscus, and the planer is inserted through the posterior internal approach to remove the posterior internal joint cavity.
Synovium. In addition, another method can also complete a total synovectomy of the posterior joint cavity. Adopt the classic approach to enter the arthroscopy. The planer is used to remove the posterior synovium between the cruciate ligament and the femoral condyle through the anterior-external or anterior-internal approach, which is beneficial for the arthroscopy to enter the posterior joint cavity and the arthroscopy to enter the posterior joint There is a certain resistance in front of the cavity, and there is a sense of breakthrough when sliding into the posterior joint space; enter the arthroscopy through the posterior internal or posterior external approach to observe the corresponding posterior space, plan the posterior synovial membrane, and then enter the lens through the posterior approach, classic approach The planer is used to plan the posterior synovium between the femoral condyle and the cruciate ligament and observe the residual synovium in the posterior joint cavity, and then enter the residual synovium from the posterior to resect. It should be noted that the planer should not face the posterior joint capsule for too long, and the attraction of the planer should not be too large, so as not to damage the popliteal blood vessels and nerves. The author reminds that total synovectomy is not a simple expansion of partial synovial resection. In particular, attention should be paid to clearing the synovium in the posterior joint cavity to avoid damage to blood vessels and nerves. The technical requirements are high and it is not suitable for beginners.
(4) Postoperative monitoring and treatment
Some surgeons believe that there is less joint bleeding after synovectomy, and drainage may not be placed. The author’s experience is that patients with total synovectomy have more blood oozing, some patients up to 500ml, it is recommended to place a closed negative pressure drainage bottle. After the operation, the affected limb is usually wrapped with thick and large burn gauze and compressed with elastic bandage. Oral non-steroidal anti-inflammatory drugs after surgery can reduce swelling, relieve pain, and increase the range of joint motion. Generally, hemostatic drugs are not used, and anticoagulants (low molecular weight heparin or rivaroxaban) are added to patients over 50 years old.
Antibiotics are used prophylactically and should be stopped within 24 hours after surgery. The quadriceps femoris isometric contraction exercise, ankle pump exercise and straight leg elevation exercise can be started the next day after the operation. On the second day after the operation, the knee joint flexion and extension activities were carried out step by step, the wound was opened and the dressing was changed, the incision condition and drainage volume were observed, and the negative pressure drainage tube was removed. The stitches are removed two weeks after surgery. Generally, the joint range of motion is required to reach 90° within one week, and over 120° within two weeks, and it should return to the preoperative range of motion 4 weeks after surgery.
Special attention should be paid to corresponding treatments according to different causes. For example, patients with rheumatoid arthritis should be treated with anti-rheumatic drugs, and patients with pigmented villous nodular synovitis should be started one month after surgery. Local radiotherapy for the knee joint, with a total dose of 1200 cGy, in 10 sessions.
(5) Prevention and treatment of common postoperative complications
1. Infection
Including wound infection and intra-articular infection, although arthroscopic surgery is less traumatic, the operation is rapid, and the flushing of the perfusion fluid significantly reduces the infection rate, but there is still the possibility of infection. Current research shows that the incidence of infection after arthroscopy is 0.5% to 0.8%, and the principle of sterility must be strictly controlled to prevent infection. The preoperative disinfection must be thorough.
The lower extremity surgery must be strictly disinfected from the part below the tourniquet to the toes. It is not possible to disinfect the knee and surrounding area according to the open surgery and then use the sterile middle to wrap the foot, because the liquid can leak to the outside. The sterile towel covering the feet is wet and contaminates the operation area. After the operation table is laid, waterproof measures should be added. Generally, a disposable sterile waterproof sheet is used for another layer.
If the operation time is long, antibiotics can be used preventively during the operation. Rapid operation, shortening the operation time, thorough flushing, effective hemostasis during the operation, and prevention of postoperative intra-articular hematoma are also effective measures to prevent infection. At the same time, the surgeon should also take sterile waterproof measures and wear waterproof clothes and shoes.
Postoperative white blood cell count increased, skin temperature of the affected limb increased, blood C-reactive protein and red blood cell sedimentation rate increased significantly. Bacterial culture and drug susceptibility test should be done quickly, antibiotics should be used empirically, and sensitivity should be selected after the drug susceptibility results come out. antibiotic. If there is no improvement after 3 days of antibiotic treatment, arthroscopic lavage and drainage can be performed urgently.
2. Postoperative bleeding and intra-articular hematoma
It is more common in operations where there are more soft tissue treatments during the operation, such as the release of the lateral knee joint support band under arthroscopy, the release of adhesions, and synovectomy. The use of high-frequency electrosurgical knife and radio frequency vaporizer for operation and intraoperative hemostasis can effectively prevent postoperative bleeding. At the same time, a negative pressure drainage tube should be placed in the joint cavity when performing this type of hand length to lead out the blood. Postoperative measures such as applying pressure on gauze layer by layer, bracing, and local cold compress are more effective. For patients with hemophilic arthritis, attention should be paid to timely supplementation of coagulation factors to normal levels before and after surgery.
3. Lower extremity venous thrombosis and pulmonary embolism
Deep vein thrombosis of the lower extremities may occur after arthroscopy. AANA’s statistics report that the incidence rate is 0.1%. Pulmonary embolism occurred in some cases, which eventually led to death. Clinicians should attach great importance to it. When the lower limbs are obviously swollen, B-ultrasound examination of blood vessels can be used to confirm the diagnosis. In terms of prevention, the tourniquet usage time should be shortened during the operation to no more than 90 minutes. After the operation, early movement of the affected limb and ankle pump exercises are encouraged. For 50-year-old patients, use low-molecular-weight Nieparin or Rivaroxaban to prevent thrombosis.
4. Tourniquet paralysis
It is related to the use of the tourniquet for too long. If the tourniquet is used for more than 90 minutes, tourniquet paralysis is more common. It is more likely to occur when the tourniquet is loosened and then continue to be applied. In mild cases, postoperative paralysis can be restored within 3 days to 3 weeks. Muscles and nerves are organically damaged and difficult to recover. Therefore, effective preventive measures can shorten the tourniquet time. The first time the tourniquet is applied does not last more than 90 minutes. The surgeon should try to complete the operation during this period. If it is really difficult, the tourniquet should be applied at least 15 minutes later.
5. Stiff joint adhesion
Joint adhesions and stiffness can occur after arthroscopy. Reasonable functional exercise rehabilitation in the early postoperative period can effectively avoid joint adhesion. If the adhesion is severe and the knee joint stiffness obviously affects the movement, arthroscopic lysis is feasible.
(6) Clinical effect evaluation
Synovectomy for rheumatoid patients has a definite preventive protective effect on the joints, and the patients can obtain satisfactory results, and joint pain and inflammation are significantly alleviated. Therefore, for patients with persistent joint swelling and hyperplasia and X-ray manifestations of 0 to I stage, medical treatment for 6 to 12 months is invalid. Only patients with synovial lesions that do not affect the joint space should be actively treated for pigmented villous nodules.
Synovitis is divided into two types: diffuse and localized. For patients with limitations, studies have shown that the postoperative effect is good, no matter whether open surgery or arthroscopic surgery, there is no recurrence after local surgery; for diffuse patients, postoperative recurrence is prone to recurrence, with a recurrence rate of 9% to 14%, surgery is recommended Local radiotherapy in the next month can greatly reduce the recurrence rate.
After total synovectomy for hemophilic arthritis, it is reported in the literature that it can reduce the number of joint bleeding, alleviate the condition and slow the progression of the disease. Patients with synovial chondromatosis underwent arthroscopic surgery, and the surgical effect is better than simple free body removal.
(source:internet, reference only)
Disclaimer of medicaltrend.org



