Macintosh laryngoscope and GlideScope laryngoscope
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
Macintosh laryngoscope and GlideScope laryngoscope under bedhead elevation
Macintosh laryngoscope and GlideScope laryngoscope under bedhead elevation. Comparison of Macintosh laryngoscope and GlideScope laryngoscope under bedhead elevation: a randomized, controlled, non-inferiority trial.
Tube intubation and difficult airway are unavoidable topics in clinical anesthesia. In view of the difficulty of 100% prediction of difficult airway and the possible serious consequences caused by difficult airway, choosing a suitable position can increase the success rate of intubation and reduce complications. The occurrence of disease is particularly important.
It is estimated that about half of difficult endotracheal intubations are not predicted and can lead to serious consequences. In order to improve the success rate of tracheal intubation, the patient’s position before intubation is very important. The most widely accepted position for tracheal intubation is the olfactory position, which has been included in the “2015 Adult Accidental Difficult Intubation Management Guidelines” published by the Difficult Airway Association. Ten years ago, Lee et al.’s study compared the effects of bed head elevation 25° and supine position in patient intubation, and introduced a new intubation position.
They found that an elevated bedside provided better throat exposure. After this groundbreaking study, other studies have found that implementing an effective bedside elevation (BUHE) during endotracheal intubation (ETI) can increase the success rate of intubation, reduce airway complications, reduce auxiliary operations, and intubate The time is shortened and the safe suffocation time during intubation is extended. At the same time, in the past ten years, the use of visual laryngoscope (VAL) equipment has increased exponentially. A large number of documents have shown that the use of visual laryngoscopes is associated with better laryngoscopy and higher exposure in patients with difficult tracheal intubation.
The success rate is related. Although the use of video laryngoscope is becoming more and more common, its high cost and fragile characteristics make it unable to be used for all patients receiving endotracheal intubation, especially in developing countries. What is the effect of BUHE position and supine position on endotracheal intubation guided by video laryngoscope? The article “Comparison of Macintosh Laryngoscopy in Bed-up-Head-Elevated Position With GlideScope Laryngoscopy: A Randomized, Controlled, Noninferiority Trial” published in Anesth Analg magazine by Tsan et al. answers this question.
Purpose
The study conducted a non-inferiority trial to compare the effects of BUHE Macintosh laryngoscope and supine GlideScope (GLSC) laryngoscope on intubation. The main purpose is to determine whether the laryngeal exposure under BUHE Macintosh laryngoscope is low. For GLSC laryngoscope. We assume that when the non-inferiority range is within −15%, the intubation of the Macintosh laryngoscope in the BUHE position can provide no less than the exposure of the larynx when the GLSC laryngoscope is used in the supine position.
Methods
Experiment method
This study was approved by the Medical Research Ethics Committee of the University of Malaya Medical Center (MREC ID No: 2017112-5770), and informed consent was obtained from all subjects before enrollment. The trial was registered on ClinicalTrials.gov before patient recruitment (Registration ID: NCT03357679, Principal Investigator: S.E.H.T, Registration Date: November 30, 2017). This study followed the Comprehensive Reporting Test Standard (CONSORT) for non-inferior randomized trial reporting.
Research objects
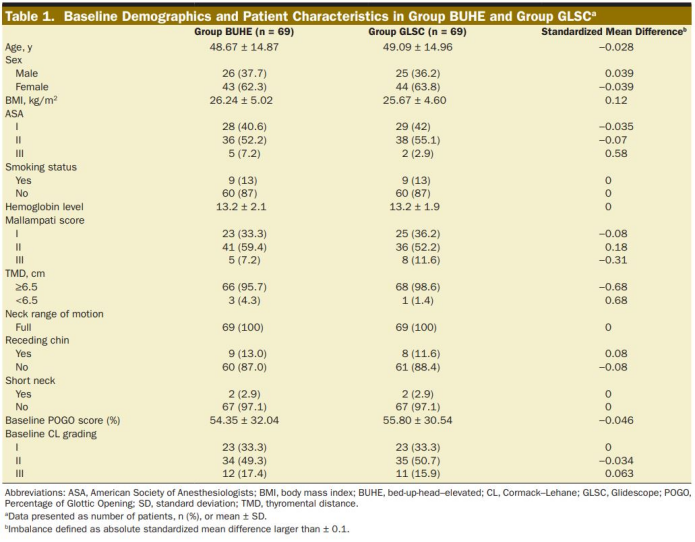
From December 2017 to September 2018, ASAI-II patients who plan to undergo elective surgery under general anesthesia and endotracheal intubation. Exclusion criteria include: ischemic heart disease, cerebrovascular disease, respiratory system disease, or BMI>35 kg·m−2. In addition, exclude patients who need fast induction or have contraindications such as airway obstruction, restricted mouth opening, or abnormal neck extension. The eligibility criteria for recruiting patients are similar to the study done by Choi et al. That is, GLSC intubation has advantages in laryngeal exposure compared with Macintosh laryngoscope intubation. The difference is that ASA III patients are included and the upper age limit of patients is 75 years old. The research subjects of Choi et al. were 15-60 years old who received GA and ASA I-II patients. The exclusion criteria were chin-jaw distance <5cm, Mallampati classification ≥3, mouth opening <3cm, restricted neck extension, front teeth sudden. Before the operation, record baseline demographic data and airway measurement data, such as the distance between nails and jaws (TMD), range of motion of the neck, short neck or mandibular retraction, and the Mallampati classification modified by Samsoon and Young.
Randomization
This is a randomized, controlled, single-blind study comparing the laryngeal exposure of the BUHE Macintosh laryngoscope and the supine GLSC laryngoscope. Computer-generated sequences were used and randomly divided into 2 groups. The study participants were divided into BUHE Macintosh laryngoscope group (BUHE group) and supine GLSC laryngoscope group (GLSC group). In the allocation concealment method, an independent researcher ((S.G.) puts the random sequence in an envelope, sealed, and numbered accordingly. The next available envelope is placed on the folder of the next enrolled patient and opened before anesthesia induction.
Before the start of anesthesia, all patients in the operating room were routinely monitored, including mean arterial pressure (MAP), heart rate, oxygen saturation (SpO2), end-tidal carbon dioxide (ETCO2), and neuromuscular monitoring. 15 patients used a standard 4.5 cm Oasis head ring (Trulife Group Ltd, Dublin, Ireland) in the supine position, and confirmed that they were in the olfactory position (SSP) by raising the occipital bone and flexion of the lower cervical spine, and straightening the head of the atlanto-occipital joint. . Both groups of patients were pre-oxygenated to induce anesthesia until the end-tidal oxygen concentration reached 85%, and then intravenously injected fentanyl 2μg·kg-1 and propofol 2-3 mg·kg-1 until the speech response disappeared. Subsequently, intravenous injection of rocuronium 0.6-1.2 mg·kg-1 or atracurium 0.5 mg·kg-1, the attending anesthesiologist decides the type of muscle relaxant used. After induction of anesthesia, face mask ventilation with 100% oxygen and 2% ~ 3% sevoflurane. A TOF-Watch neuromuscular monitor (Organon Ltd, Dublin, Ireland) was used to determine the degree of neuromuscular relaxation until the four TOFs of the ulnar nerve were stimulated and disappeared.
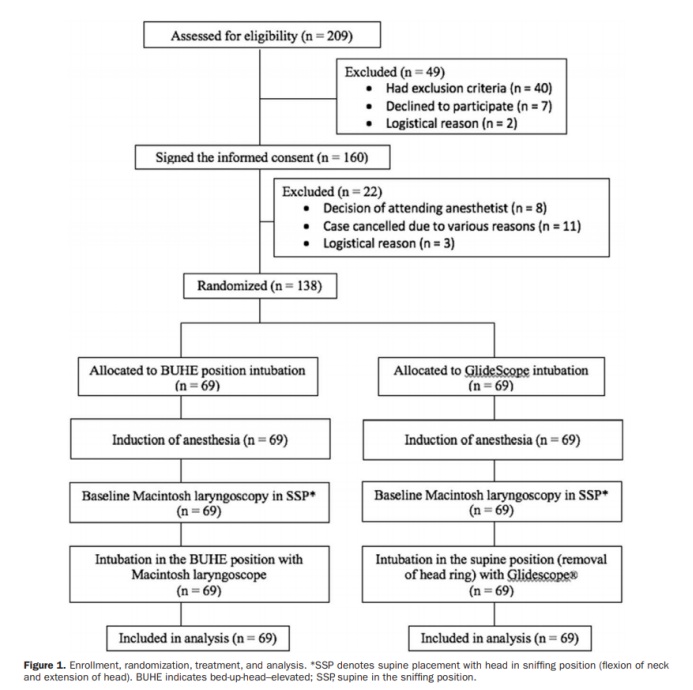
Subsequently, 1 of the 2 researchers (SML and MFZA) who did not know the patient group (using No. 3 or 4 Macintosh laryngoscopes for benchmark laryngoscopy, quantified and recorded the exposure of the larynx. In the benchmark larynx After the endoscopy, take the corresponding position according to the patient’s group. The BUHE position is adopted for the patients in the BUHE group, that is, the headboard of the operation bed is raised to raise the headboard of the bed by 20°~30° until the patient’s external auditory canal is level with the sternum angle. An investigator (SEHT) used a 3 or 4 Macintosh laryngoscope for positioning, intubation, and laryngeal exposure assessment. At the same time, the investigator (SEHT) independently inserted the GLSC LoPro T3 laryngeal lens in the supine position (with the head ring removed). The researcher has done more than 50 GLSC intubations before. Figure 1 summarizes the research status of all patients. All researchers have more than 5 years of experience in anesthesia and intensive care units. Need to try intubation again and perform mask oxygenation with manual balloon. Failure of intubation is defined as failure of intubation after 3 attempts, and the patient will be treated in accordance with the department’s difficult airway guidelines.
Observation index
The main measurement result is the exposure of the larynx, expressed as a percentage of the Glottis Openness (POGO) score. A POGO score of 100% means that the entire glottis opening from the front of the vocal cords to the interddle notch can be seen. A POGO score of 0% means that the throat structure is completely invisible. In addition, laryngeal exposure is also assessed by the Cormack-Lehane (CL) classification of the glottis. The larynx exposure was measured in the baseline olfactory level and the intervention group. The investigator who assessed the larynx exposure at the baseline olfactory level was blind to the larynx exposure of the intervention group, and vice versa, and the two recorded the larynx exposure separately.
Secondary outcome indicators, including intubation time (TRI), number of intubation attempts, use of airway aids, need for extralaryngeal manipulation, difficulty in intubation (based on visual analogue score, 0 means no difficulty, 10 means very difficult) And complications during intubation (esophageal intubation, hypoxia, hypotension). The intubation time is defined as the time from the laryngoscope lens tip (passing the incisor to the first detection of ETCO2 (in seconds), recorded by another anesthesiologist who did not participate in this study. Hypoxia is defined as SpO2 <92%, hypotension is defined as MAP <60mmHg.
Statistical Analysis
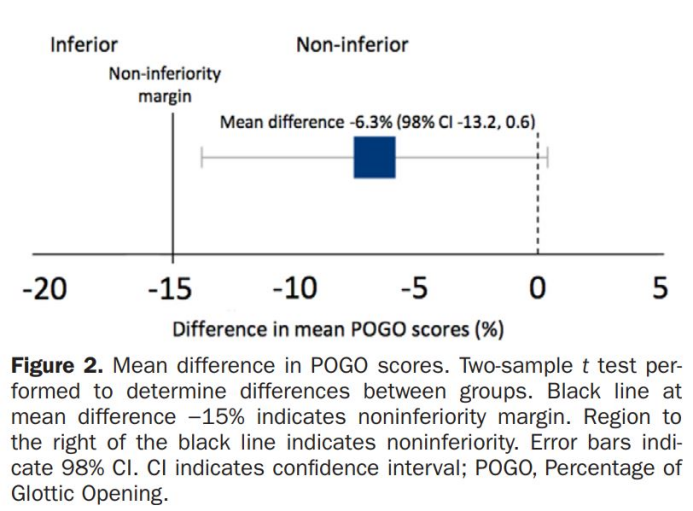
Based on research data from patients planning to undergo elective surgery, the GLSC laryngoscope was compared with a normal Macintosh laryngoscope. Compared with the Macintosh group, the POGO score of the GLSC group increased by an average of 22.00% (95% confidence interval [CI], 10.63-33.67). Based on the significant difference in the POGO score, we set the clinically significant non-inferiority range to 15%, because a small difference does not significantly improve the larynx exposure, nor does it increase the success rate of endotracheal intubation , And a large difference may turn direct intubation into difficult intubation.
The main results used 0.01 α level and two-sided 98% (100 × {1-2α}) confidence interval to test the non-inferiority of the lower limit of CI. If the lower limit of 98% CI is higher than the set lower limit of -15% non-inferiority, it will be considered non-inferiority. For secondary results, a 2-sample t test was used to evaluate the superiority of continuous variables, and a Pearsonχ2 test or Fisher’s exact test was used for categorical variables (the conditions of Pearsonχ2 test were not met).
Mann-Whitney test is used for continuous data variables with non-normal distribution. Paired t test was used to test the difference between the POGO score of the intervention group and the baseline POGO score of the olfactory level group. The Shapiro-Wilk test was used to evaluate the normal distribution of continuous variables. All statistical analyses were performed using SPSS version 22.0 (SPSS Inc, Chicago, IL). According to the research protocol, there are 10 superiority tests (8 secondary comparisons between groups and 2 baseline comparisons within groups). The Bonferroni method was used to adjust the significance standard to maintain the type I error rate α at 0.05. The two-sided P value has 90% statistical power, and the α level is 0.01 to test the non-inferiority hypothesis. According to previous studies, the estimated standard deviation (SD) of the POGO scale is 22%. The calculated sample size includes a dropout rate of 20%, and the study requires a minimum of 137 patients.
The results
A total of 138 ASA I-III patients were recruited in this study, and all patients were included in the study for intentional analysis. Except for the higher BMI in the BUHE group and a higher proportion of patients with ASA III, Mallampati 2 and TMD <6.5 cm, the baseline characteristics of the BUHE group (n = 69) and the GLSC group (n = 69) were similar. There was no clinically relevant difference between the BUHE group and the GLSC group in the baseline POGO score of the laryngoscopy in the olfactory position and the baseline CL classification of the two groups of patients (Table 1).
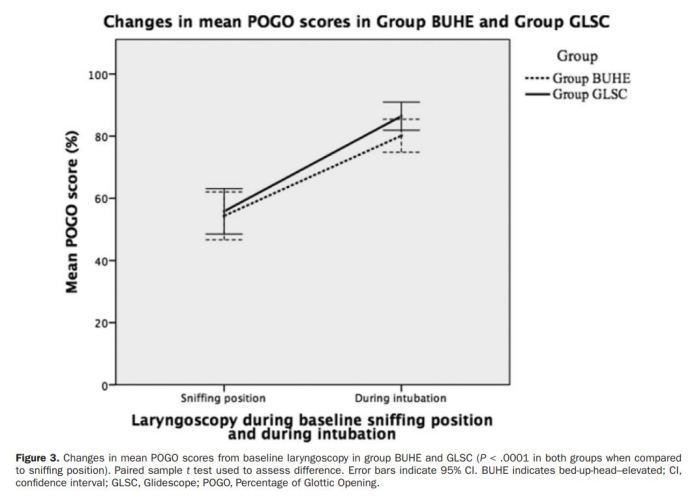
At the time of intubation, the POGO scores of the BUHE group and GLSC group were 80.14%±22.03% and 86.45%±18.8%, respectively (Table 2).
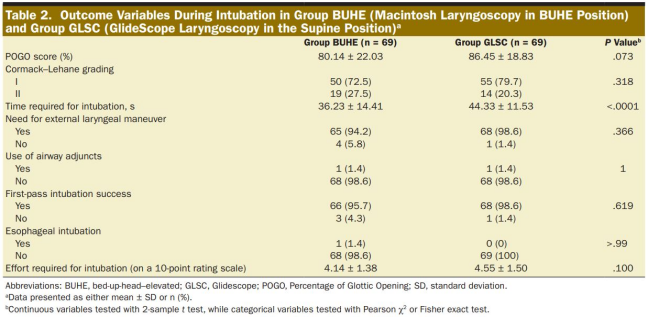
The difference in POGO scores between the two groups was −6.3% (98% CI, −13.2% ~ 0.6%). When the non-inferiority range is set to −15%, the exposure of the larynx at the BUHE position is no less than that of the GLSC laryngoscope (Figure 2).
Compared with the POGO score of the baseline laryngoscopy at the sniffing position, the POGO scores of the two groups were significantly higher (BUHE group: 25.80%; 95% CI, 20.89-30.70, GLSC group: 30.65%; 95% CI, 23.90-37.40; P <.0001 in both groups; Figure 3). There was no significant difference in CL classification between the two groups after the intervention.
The intubation time of the BUHE group (36.23±14.41 seconds) was significantly shorter than that of the GLSC group (44.33±11.53 seconds), and the average difference was 8.1±4.2 seconds (P <.0001). There were no significant differences between groups in other secondary results (Table 2). 3 patients (4.3%) in the BUHE group and 1 patient (1.4%) in the GLSC group failed the first intubation, but both succeeded in the second intubation attempt. There was no significant difference in the degree of difficulty in the intubation process between the two groups (P = 0.1). No hypotension or hypoxia occurred in the two groups.
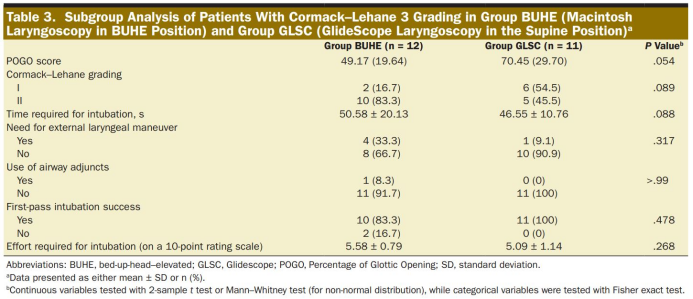
Post hoc analysis was performed on patients in the BUHE group (n = 12) and GLSC group (n = 11) with a baseline CL of grade 3 (usually classified as difficult intubation) (Table 3). The POGO scores of the two groups were compared with baseline. There is a significant improvement (P <0.0001). The GLSC group (70.45%±29.70%) and the BUHE group (49.17%±19.64%) had no significant difference in the mean of POGO scores (P = 0.054). There were no significant differences between the two groups in intubation time, auxiliary operations, use of airway aids, success rate of first intubation, and difficulty in intubation
Disccusion:
This is the first study to compare the GLSC laryngoscope in the supine position with the BUHE laryngoscope. Studies have shown that in the general population, when the non-inferiority margin is set to −15%, the laryngeal exposure of the BUHE laryngoscope is no less than that of the GLSC laryngoscope. Compared with the olfactory level, the use of BUHE position or the use of GLSC laryngoscope can significantly improve the POGO score. The intubation time of BUHE position is shorter than that of GLSC position.
We conducted a subgroup analysis of CL 3 patients and found that the POGO scores of the BUHE and GLSC groups were significantly higher than the baseline, making the intubation easier to succeed. Our findings support the results of other studies, that is, compared with the olfactory level, patients with GLSC laryngoscope or BUHE position intubation have significantly improved laryngeal exposure. The improvement in laryngeal exposure is not only suitable for patients with normal airways, but even for patients with potentially difficult intubation whose vocal cords are not visible (CL3).
A recent study by Semler et al. found that compared with the olfactory level, the intubation of critically ill patients in a slope position (bed elevation of 25°) increased the incidence of CL 3 or 4. This can be explained by intubation by multiple clinicians, resulting in a higher observer deviation. The characteristics and intubation environment of the emergency intubation patients in the study are also different from those in the operating room. The conditions of the patients in the operating room are more complete and the environment is more controllable. In addition, studies have shown that even if the correlation between the POGO score and the CL score between anesthesiologists is very poor, this may be due to the inability to recall and cause the classification error.
This study uses a non-inferior experimental design. The video laryngoscope has been recommended as the standard configuration for intubation, and it is more and more widely used. However, due to cost issues, its widespread use in many hospitals around the world is impossible and impractical. Therefore, it is still necessary to further improve the Macintosh laryngoscope. Our non-inferiority trial design is based on the assumption that for all patients undergoing endotracheal intubation, the BUHE position of laryngoscope intubation is no less than visual laryngoscope, and the results support that the BUHE position can be used as a standard intubation position. As a standard intubation position, the improvement of the BUHE position on the exposure of the larynx will help all clinicians to change the difficult endotracheal intubation into a simple intubation during the endotracheal intubation process. In addition, not all clinicians can use visual laryngoscopes, making the BUHE position a not bad choice.
In our study, the olfactory position was achieved by raising the patient’s occiput through a 4.5 cm head ring and stretching the head at the atlanto-occipital joint, placing the patient in a position of “breathing the early morning air” position. Horton et al. described the olfactory level as the neck flexion 35°, the head extended 15° in the horizontal position, the head height is between 31-71mm, and the average height is 55mm. The height of the 45mm headband used by our patients is within the range described, and we visually confirm that all patients’ neck flexion and extension are consistent with the olfactory position described in the 2015 difficult airway management guidelines for unpredicted adult difficult intubation .
In general laryngoscopy, the best exposure of the larynx requires alignment of the three axes of the mouth, pharynx, and larynx. Lee et al. believe that the effect of BUHE on larynx exposure is due to gravity. In the BUHE position, directly or indirectly pulling down the upper chest structure to move the laryngeal structure to the tail end may promote the laryngeal axis to be in line with the line of sight during laryngoscopy. In addition, during BUHE laryngoscopy, the horizontal force applied has increased, while the vertical force has decreased. This is due to the change in the direction of the laryngoscope handle, which is raised 45° in the supine position and 20° in the BUHE position. Changes in force, vector, and torque, coupled with the influence of gravity, may affect the exposure of the larynx structure of the BUHE patient.
It has been confirmed that the intubation time of the GLSC group is longer than the standard intubation time under the Macintosh laryngoscope. Our study also showed that GLSC intubation takes about 8 seconds longer than BUHE intubation. Although the length of the intubation time in the operating room is not clinically significant, the shorter intubation time is an additional advantage of the BUHE position. If GLSC intubation is performed by an inexperienced person, this difference may be even greater and cause complications. There was no significant difference between the BUHE position and the GLSC position in the need for extralaryngeal operations, the use of airway aids, the success rate of the first intubation, the incidence of esophageal intubation, and the difficulty of intubation. In theory, BUHE has the disadvantage of reducing cerebral perfusion, especially in the case of hypotension. There was no hypotension in our study, it may be that the study could not detect the existence of the difference. More research is needed to determine the potential complications of BUHE. Another potential research direction is GLSC laryngoscope intubation at the BUHE position, which may improve the success rate of airway management.
This study ruled out possible airway difficulties, including patients with BMI >35 kg·m−2. The reason is that the inclusion of patients with difficult intubation characteristics may lead to the introduction of confounding factors in the analysis, and we want to evaluate whether the BUHE position Macintosh laryngoscope can be used as a standard position for general anesthesia endotracheal intubation in the general population. In addition, considering that there may be difficulties in mask ventilation, it is not ethical to re-endotracheal intubation for these patients. For the application value of BUHE position in this specific population, randomized controlled trials can be conducted in the future to compare the effects of BUHE position laryngoscope and visual laryngoscope on patients with difficult airway.
Because of the complex interaction between patient factors, environmental factors, and clinician skills, there is no standardized definition of difficult airways in the article. The difficult airway defined by ASA is more recommended, and it is described as difficult to expose the laryngoscope, that is, the glottis is not visible under the laryngoscope. Therefore, in this study, we chose the degree of laryngeal exposure as our main result, because the degree of laryngoscope exposure is an important determinant of the success of tracheal intubation. Although poor exposure of the glottis is not always associated with difficult intubation, it can also lead to difficult intubation. The Difficult Intubation Scale (IDS) regards glottis exposure as one of the influencing factors of difficult intubation, and is a more objective scale to measure difficult intubation. Therefore, when all other factors remain unchanged, improving the patient’s laryngoscope field of view will increase the success rate of intubation.
Our research has some limitations. First of all, in this study, the intubation researcher was not blind to the patient’s intubation position and method, which may lead to observer bias in the study. We tried to reduce this effect by not telling the intubation investigator of the larynx exposure of the baseline olfactory level. In addition, the investigator who performed the baseline laryngoscopy did not know the group of patients. Secondly, only one researcher performed all intubations, which may make the results of this study not universal. We accept this risk to reduce observer bias (which may produce more confounding factors). Similar to most anesthesiologists in the world, the investigator performing the intubation has ≥5 years of anesthesia experience and has performed >50 GLSC laryngoscopy. Third, when trying to extrapolate the results to different clinical settings, it must be considered that this is a single-center study.
Conclusion
Our conclusion is that in the general population, the BUHE position can provide laryngoscopy as much as the GLSC laryngoscope, and the larynx exposure obtained by both methods is better than that obtained by the olfactory level. In view of the many advantages of intubation at the BUHE position, unproven adverse reactions, ease of use, and high cost-effectiveness, we recommend that clinicians consider the BUHE position as the standard intubation position for all patients when intubating under the Macintosh laryngoscope.
Reviews
Tracheal intubation and difficult airway are unavoidable topics in clinical anesthesia. In view of the difficulty of 100% prediction of difficult airway and the possible serious consequences caused by difficult airway, choosing the right position to increase the success rate of intubation and reduce complications The occurrence of disease is particularly important. The classic intubation position is the olfactory position. For most patients, the three axes of the oropharynx can be in a straight line, but exceptions are not uncommon.
Bedhead elevation (BUHE) has been shown in multiple studies (including the above studies) to show better laryngeal exposure and shorter intubation time. The effect is similar to that of a visual laryngoscope, and there is no visual laryngoscope for underdeveloped areas. The condition of the mirror can increase the success rate of intubation and reduce the risk. But it needs to be realized that although no related complications were found in the study, it should be noted in clinical application: patients with shock and other patients whose posture may affect cerebral perfusion, patients with head and neck injuries or cervical spine diseases may not be suitable for the BUHE position. In addition, as stated at the end of the article, it is a single-center, single-blind study, and the tracheal intubation operation is performed by only one investigator.
Therefore, there are certain systematic errors. The results may not be universal, which limits its promotion. Secondly, under the premise that the penetration rate of video laryngoscope is greatly improved, the application of special position intubation may not be the best choice when reducing the risk of complications that may be caused by special positions. Third, the focus should still be on preoperative airway assessment and difficult airway screening. Detailed and comprehensive assessment and screening are the guarantee for reducing airway risks. In addition, difficult airway pre-plans and necessary preparations (such as Bronchoscopy, etc.) is also very important.
(source:internet, reference only)
Disclaimer of medicaltrend.org



