Discharged in 10 days after COVID-19+ AIDS + tuberculosis triple-infection
- Why Botulinum Toxin Reigns as One of the Deadliest Poisons?
- FDA Approves Pfizer’s One-Time Gene Therapy for Hemophilia B: $3.5 Million per Dose
- Aspirin: Study Finds Greater Benefits for These Colorectal Cancer Patients
- Cancer Can Occur Without Genetic Mutations?
- Statins Lower Blood Lipids: How Long is a Course?
- Warning: Smartwatch Blood Sugar Measurement Deemed Dangerous
Discharged in 10 days after COVID-19+ AIDS + tuberculosis triple-infection
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Discharged in 10 days after COVID-19+ AIDS + tuberculosis triple-infection.
Recently, the International Medical Case Reports Journal released a case report of triple infections of COVID-19, AIDS, and tuberculosis. The patient recovered and was discharged after 10 days of hospitalization. [1]
This case report shows that COVID-19 patients with AIDS and tuberculosis infection can have a good prognosis; in addition, patients with COVID-19 should consider the possibility of co-infection when they are admitted to the hospital, and conduct a comprehensive examination for all similar clinical manifestations.
 Case reports surviving the triple infection of COVID-19, AIDS, and tuberculosis (picture source: International Medical Case Reports Journal)
Case reports surviving the triple infection of COVID-19, AIDS, and tuberculosis (picture source: International Medical Case Reports Journal)
The patient was a 55-year-old man who was admitted to the hospital for 5 days with high fever, headache, cough, and shortness of breath. He coughed up blood and sputum 1 month ago, accompanied by loss of appetite, weight loss, chest pain, night sweats, and fatigue.
The patient was in very poor condition at the time of admission, with a body temperature of 39.3 degrees, a heart rate of 112 beats per minute, a blood pressure of 110/60 mmHg, a breathing rate of 38 breaths per minute, shallow breathing and use of respiratory assist muscles, and an oxygen saturation of 87% . There is dullness in the lower left lobe of the lung, rough crackles in the upper and lower left lobe, and blisters on the right chest, but it is greatly reduced at the base of the lung.
The patient was admitted to the hospital urgently for oxygen inhalation through a nasal cannula.
Can be cured with conventional treatments
According to routine laboratory examinations performed after admission, the patient has an increase in white blood cells, mainly lymphocytes, and an increase in red blood cell sedimentation rate. Bacterial biofilm (BF) does not contain hemoglobin, liver and kidney functions are normal, random blood sugar is normal, and a plain chest film shows peripheral patchy shadows.
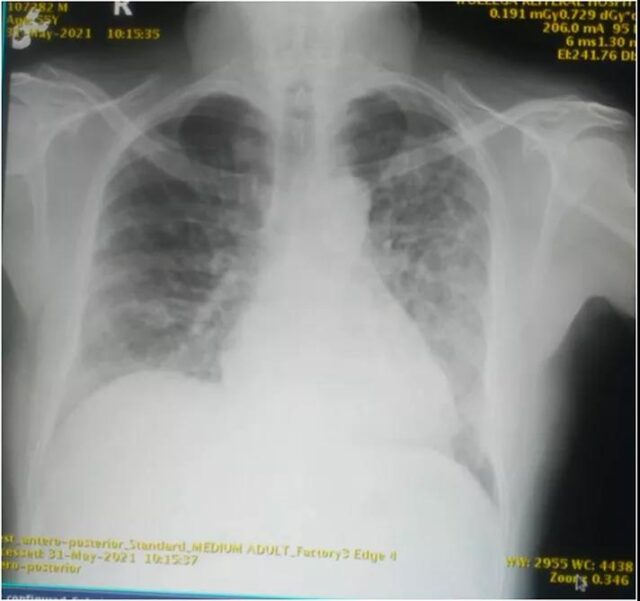
Plain chest radiograph showing peripheral flaky shadows (Image source: International Medical Case Reports Journal)
The patient has a history of AIDS for 3 years, regularly undergoes antiretroviral therapy (TDF 300 mg + FTC 200 mg + EFV 600 mg), CD4 T cell count at admission is 266 cells per cubic millimeter, and HIV-1 RNA level is 9000 copies per milliliter .
When the patient was admitted to the hospital, the COVID-19 nucleic acid test of the nasopharyngeal swab was positive. However, AIDS patients may have multiple co-infections due to a weak immune system. After a comprehensive examination, the sputum test results on the day of admission showed that the nucleic acid test of Mycobacterium tuberculosis was positive.
On the first day of admission, the doctor asked the patient to continue the pre-admission antiretroviral therapy to treat AIDS, in addition to routine fluid management and empirical antibiotics (cefepime), and oxygen inhalation through a nasal catheter to keep the patient’s blood oxygen saturation at 92-96%, while giving patients 6 mg of dexamethasone daily, closely monitor vital signs, breathing and mental status.
On the 3rd day of admission, RHZE (rifampicin, isoniazid, pyrazinamide, and ethambutol) was started for anti-tuberculosis treatment.
On the 6th day of admission, the patient’s fever subsided, and the general condition improved. At this time, the COVID-19 test result was negative, and the blood oxygen saturation could be kept above 94% in indoor air.
On the 10th day of admission, the patient was discharged, and then continued antiretroviral and antituberculosis treatment in the outpatient clinic for 2 weeks.
The case report believes that the reason why the patient recovered so quickly may be due to strict early compliance with antiretroviral and anti-tuberculosis treatment, but further research is needed to prove the rationality of this.
Co-infection may not aggravate COVID-19
The results of a limited number of studies from 2019 to the present indicate that tuberculosis may increase the susceptibility and severity of COVID-19, while AIDS may not.
Regarding the impact of tuberculosis on COVID-19, a systematic review integrated 113 related articles and concluded that “patients with comorbidities have a higher risk of death”. Among these articles, only 8 articles have clinical details of tuberculosis patients with COVID-19disease, a total of 10 cases. [2]
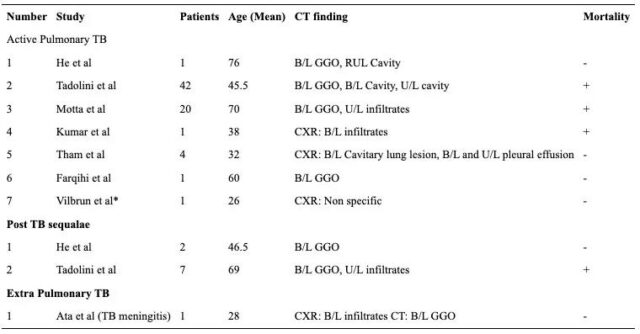
10 patients’ age, CT appearance, mortality and other information, Image source: Acta Biomed
According to the results of a representative study, a report from Liaoning, China showed that 36% of patients with COVID-19 have a history of tuberculosis, which is significantly higher than other complications. Tuberculosis infection may increase the susceptibility and severity of COVID-19. [3] A report of 49 patients with tuberculosis and COVID-19 from 8 countries showed that one-third of COVID-19 infections were detected during tuberculosis treatment, and that among elderly patients with COVID-19 and tuberculosis, the mortality rate higher. [4]
It is controversial as to whether AIDS co-infection will increase the re-coronal condition.
In a large-scale observational study in South Africa, HIV-positive patients with COVID-19 more than doubled their chances of death. Regardless of the HIV-related viral load or degree of immunosuppression, the increased risk of death remained unchanged. [5] Data from a British study showed that compared with people without HIV, the risk of HIV infection with COVID-19 has nearly tripled. [6]
However, according to the COVID-19 Survey of AIDS Patients in Two Districts of Wuhan, China, the incidence of COVID-19 among AIDS patients is comparable to that of the general population. [7] According to a German study, only 9% of 32 AIDS and COVID-19 dual infections died, of which 76% were mild. [8] An Italian study found that people with dual infections of AIDS and COVID-19 have a 96% survival rate. [9]
Regarding the reasons why AIDS does not increase COVID-19 re-infection, Italian research believes that antiretroviral therapy may play a role in the good prognosis of COVID-19; [9] A Spanish study believes that anti-retroviral enzyme inhibitors can protect patients Not infected with COVID-19. [10]
First death: the cause may be poorly controlled AIDS
In fact, 4 cases of this triple infection of COVID-19, tuberculosis and AIDS were reported in August last year, of which 2 were in Brazil[11] and 2 were in Panama[12], all recovered and discharged within 2 months.
However, in June 2021, Colombia had the world’s first death of a triple infection of COVID-19, tuberculosis, and AIDS. [13]
The patient was a 34-year-old woman who presented to the doctor with fever, dyspnea and headache. A history of AIDS for 6 years, irregular treatment, and a history of illegal drug abuse (marijuana and cocaine). The patient presented with moderate to severe dehydration and mild respiratory distress on admission. The respiratory rate was 28-30 breaths per minute, the oxygen saturation was 85-90%, and the heart rate was 108 beats per minute. Chest CT showed bilateral pleural effusion, diffuse shadows in both lungs, ground glass degeneration in the lower left lobe, and two pulmonary nodules.
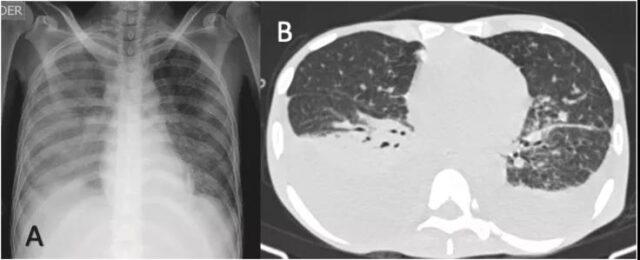 Chest radiography and CT, Image source: NCBI
Chest radiography and CT, Image source: NCBI
The doctor gives the patient mechanical ventilation and uses hormones (deoxycorticosterone) and antibacterial drugs (ampicillin, sulfa, doxycycline). However, the patient’s condition deteriorated, his dyspnea worsened, and he died on the second day of hospitalization.
This case report believes that the patient’s worsening condition may be due to: the patient did not adhere to antiretroviral therapy, low CD4 T cell count, high viral load, hypoalbuminemia, lymphopenia, and increased acute phase reactants , The diagnosis of tuberculosis is late.
When the patient in this death case was admitted to the hospital, the CD4 T cell count was 25 per cubic millimeter, and the HIV-1 RNA level was 910,000 copies per milliliter. The AIDS control situation was far worse than that of the five recovered patients. (Content review: gyouza)
Expert Comments: Discharged in 10 days after COVID-19+ AIDS + tuberculosis triple-infection.
With the rapid increase in the number of COVID-19 infections worldwide, the number of COVID-19 infections with various underlying diseases is also an inevitable trend. Many studies have focused on the severe incidence and mortality of people with different underlying diseases after being infected with the COVID-19 virus.
On the other hand, HIV is an important reason for the resurgence of tuberculosis. HIV combined with tuberculosis is the most common opportunistic infection of HIV-infected people in many countries. Advances in HIV treatment have allowed more infected people to survive for a long time, and HIV-infected people are just like ordinary people. Will encounter various acute and chronic diseases.
There have been more reports of HIV-infected people co-infecting with the new coronavirus. For HIV-infected people who have been treated regularly and have better virus control, the prognosis after infection with the new coronavirus is not significantly different from that of the general population of the same age.
HIV infection in some areas The increased susceptibility of patients to the new coronavirus and the mortality rate after infection may be related to the low HIV antiviral coverage and poor treatment effects in the local area.
This article focuses on AIDS combined with tuberculosis and re-infection with new coronavirus. Part of the poor prognosis should also be due to poor HIV control of HIV-infected people with tuberculosis, high viral load, low CD4 level, and decreased immune function The population is highly susceptible to the new coronavirus and the prognosis is poor.
If HIV-infected people do not receive effective treatment, the effect of immunization with the COVID-19 vaccine after the immune function declines may also be worse than that of people with normal immune functions, and it may also increase the susceptibility of HIV-infected people to the COVID-19 virus and increase the incidence of severe illness after infection.
Therefore, the research results suggest that we should actively give HIV-infected people effective antiviral treatment to maintain the immune function at a normal level, which can reduce the incidence of various opportunistic infections including tuberculosis, and active vaccination of the COVID-19 vaccine can reduce the COVID-19 virus Susceptibility and incidence of severe illness after infection.
Discharged in 10 days after COVID-19+ AIDS + tuberculosis triple-infection.
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



