Why are more and more women choosing to have their healthy fallopian tubes removed?
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
Why are more and more women choosing to have their healthy fallopian tubes removed?
- Red Yeast Rice Scare Grips Japan: Over 114 Hospitalized and 5 Deaths
- Long COVID Brain Fog: Blood-Brain Barrier Damage and Persistent Inflammation
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Why are more and more women choosing to have their healthy fallopian tubes removed?
The number of prophylactic bilateral salpingectomies performed during benign gynecologic surgery is increasing.
The reason behind this is that there is still a lack of effective screening methods and early diagnosis strategies for ovarian cancer, and 70% of patients are found at an advanced stage.
Recently, the non-profit international organization “Ovarian Cancer Research Alliance (OCRA)” launched a “Cancer Prevention Action”. One of the contents is to encourage women to preventively remove both fallopian tubes during pelvic surgery.
The agency pointed out that 70% of ovarian cancers start in the fallopian tube, and preventive removal of it has been proven to significantly reduce the risk of cancer.
Epidemiological surveys show that the lifetime risk of ovarian cancer for ordinary women is about 1.5%, much lower than breast cancer (12.5%). However, the 5-year survival rate of ovarian cancer hovers at 40%, and the mortality rate is high.
“Global Cancer Statistics 2020” shows that there were 55,342 new cases of ovarian cancer in China that year, and 37,519 deaths.
“Prophylactic removal of the fallopian tubes may be a win-win. It reduces the risk of ovarian cancer, but also preserves the ovaries and continues to produce the hormones the body needs.” Dianne Miller, director of the Department of Gynecological Oncology, Obstetrics and Gynecology, University of British Columbia, Canada ) said that in the local area, this is already a routine operation.
In September 2010, the British Columbia Ovarian Cancer Research Organization launched the “Provincial Gynecologist Education Program”, hoping that doctors will perform bilateral salpingectomy when performing permanent contraceptive operations such as hysterectomy and tubal ligation.
The following year, the Canadian Society of Gynecologic Oncology issued a statement acknowledging the cancer-preventive potential of prophylactic removal of the fallopian tubes.
However, the medical profession still adopts a cautious attitude towards this procedure. Many experts believe that the timing of surgery and age considerations are very important.
Overemphasis on preventive surgery may induce anxiety and divert medical resources. Considering surgical complications and late effects, women must have in-depth communication with clinicians.
Ovarian cancer is too difficult to detect early
Gynecological cancers have characteristics such as heredity and familial clustering. Studies have shown that if someone in the family suffers from ovarian cancer, the risk of cancer in female relatives is several times that of ordinary people.
One of the reasons behind this is that mutated genes such as BRCA are passed on from generation to generation.
BRCA1 and BRCA2 are important tumor suppressor genes that produce proteins and repair damaged DNA. Any mutation related to it may increase the instability of the gene, thereby increasing the risk of breast cancer and ovarian cancer.
At present, there are about 20 genetic susceptibility genes related to ovarian cancer, among which BRCA has the most significant influence.
BRCA1/2 germline mutation carriers have a lifetime cumulative risk of developing ovarian cancer of 54% and 23%, respectively, making them a high-risk population for ovarian cancer.
American movie star Angelina Jolie is a BRCA1 mutation carrier. She had her breasts, ovaries and fallopian tubes removed preventively in 2013 and 2015, respectively. But unlike Jolie, OCRA’s recommendation to remove the fallopian tubes is aimed at the “general risk” population, that is, those who do not carry risk factors such as mutated genes and family history—it can be understood as “every woman with ovaries.”
Breast cancer has a variety of early screening methods, such as breast ultrasound, X-ray examination, magnetic resonance (MRI) and so on. According to the results of multiple prospective RCT clinical trials, effective screening can reduce the mortality rate of breast cancer by 20%.
Unfortunately, so far, there is still a lack of effective screening methods and early diagnosis strategies for ovarian cancer in the world, and 70% of patients are diagnosed at an advanced stage.
In 2021, the United Kingdom released a study of 200,000 people. It was believed that transvaginal B-ultrasound and serum carbohydrate antigen (CA) 125, which had been expected earlier, were not satisfactory.
Neither alone nor in combination can achieve the effect of early detection of ovarian cancer and ultimately reducing the mortality rate of ovarian cancer in the population.
In 2018, the U.S. Preventive Services Task Force issued a statement stating that ovarian cancer screening for general risk groups cannot reduce ovarian cancer mortality, and false positive results in screening will increase moderate to severe harm.
Combined screening of transvaginal B-ultrasound and serum carbohydrate antigen (CA) 125 is currently mainly used for high-risk groups, including those carrying BRCA1/2 germline mutations, ovarian cancer, breast cancer, Lynch syndrome, Leigh-Fraumeni Syndrome history or family history.
“There are cancer patients under the age of 50 in the family, which tends to be familial tumors.
For high-risk groups, it is recommended to perform genetic testing, genetic counseling, and risk assessment first, and at the same time give recommendations for strengthening relevant cancer screening. “
BRCA1 mutations are recommended to be performed at the age of 35-40 after childbearing, and BRCA2 mutations are recommended to be performed at the age of 40-45 after childbearing.
If there is an existing case with the same mutation in the family, the timing of prophylactic resection should be earlier than the age of onset of the case.
Who needs to have their fallopian tubes cut?
“In the past 10 years, gynecologists have performed more salpingectomy in hysterectomies of average risk patients. Part of the reason is that ovarian cancer is difficult to detect early and requires surgical prevention.” Department of Obstetrics and Gynecology, Duke University School of Medicine, USA Professor Evan R. Myers said.
Preventive salpingectomy for the general population must be carried out at the same time as other gynecological operations. There are mainly 4 situations in which women are mobilized for this procedure:
- First, when patients with benign gynecological diseases need hysterectomy;
- Second, for those who have no future fertility requirements, when removing uterine fibroids and ovarian cysts;
- Third, severe complications are found during cesarean section and permanent sterilization is required; fourth, when the ovaries need to be removed due to illness.
From a practical point of view, the operation will remove the fallopian tubes as completely as possible. The whole process only takes more than 10 minutes, and generally does not increase the risk of infection and bleeding.
If the person who simply removed the fallopian tubes wants to have a child again in the future, he can use assisted reproductive technology to fulfill his childbearing desire.
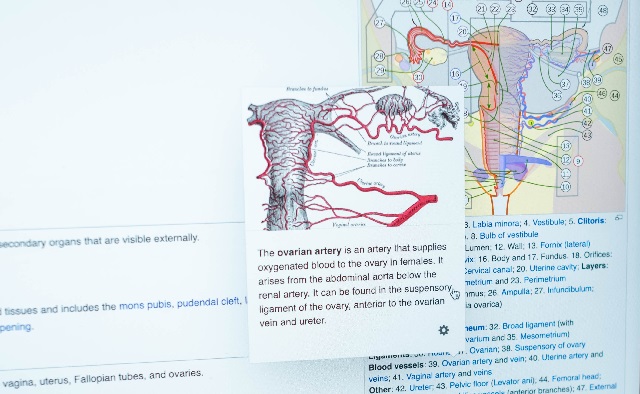
There is increasing evidence that high-grade serous epithelial ovarian cancer originates in the fallopian tube and is directly related to the mucosal cells at the fimbria of the fallopian tube.
For the general population, complete resection of the fallopian tubes is recommended for those who have the opportunity for pelvic surgery and have no fertility requirements. Where it is not possible for anatomical or technical reasons, it also makes sense to cut as many as possible.
Surgery is more extensive for people who are at high risk of hereditary ovarian cancer.
In February 2022, a sub-journal of JAMA published a cohort study of nearly 60,000 women in British Columbia, Canada. The results showed that the incidence of epithelial ovarian cancer in the preventive resection group was much lower than that in the control group. A Swedish study reported a 65% reduction in the risk of ovarian cancer in the preventive resection group.
However, for things that seem to have clear benefits, many interviewees believe that they should be carefully considered, “the most afraid of patients regretting it.”
On the one hand, prophylactic salpingectomy is a risk-reducing operation, but it cannot completely eliminate cancer.
Preventive removal of fallopian tubes can mainly reduce the risk of common epithelial cancer, and has limited impact on the prevention of other types of ovarian cancer.
Comprehensive studies have reported that in high-risk groups carrying mutated genes, after both ovaries and fallopian tubes are removed, the relative risk can be reduced by 75%-96%.
On the other hand, salpingectomy may have an impact on ovarian blood supply. “Potential adverse effects on ovarian functional reserve” of the procedure.
Adnexectomy, especially around menopause, can lead to iatrogenic estrogen deficiency and an increased risk of coronary heart disease, stroke, hip fracture, Parkinson’s disease, cognitive impairment, depression, and anxiety.
Also, the effect of salpingectomy alone is minimal. Relatively speaking, hysterectomy has a relatively greater impact on ovarian blood supply, and may cause ovarian function to decline 1-2 years in advance.
If you want to prevent cancer by hysterectomy and ovarian cancer at a young age, you must be extra cautious.
Surgical volume is increasing across countries
“When performing benign gynecological surgery, the number of prophylactic bilateral salpingectomy is increasing.” In April 2019, the American College of Obstetricians and Gynecologists (ACOG) updated relevant guidelines on the benefits and feasibility of prophylactic salpingectomy And long-term follow-up, etc., and put forward relevant recommendations again.
Its content shows that a survey of ACOG member doctors found that 77% of patients were already carrying out preventive bilateral salpingectomy when undergoing hysterectomy to screen and reduce the risk of ovarian cancer.
The proportions of preventive surgery during postpartum permanent sterilization and caesarean section were 26% and 37%, respectively.
Some Asian countries are also actively carrying out related surgeries. In 2018, the Korean Society of Obstetrics and Gynecology issued a position statement on prophylactic salpingectomy, stating that it is safe and feasible. In 2019, a survey of Japanese doctors showed that 28% (n=19/68) would perform preventive salpingectomy during caesarean section.
In March 2020, Japan announced that preventive ovaries and salpingectomy for patients with BRCA germline mutations and a family history of cancer will be included in the national medical insurance.
The number of cases of prophylactic salpingectomy in China is unknown. There is limited discussion of its clinical feasibility in Chinese academic journals.
Some analysts pointed out that China’s medical resources for familial hereditary tumor research and genetic testing are mainly distributed in first-tier cities.
Women in remote areas have no awareness of early screening, and it is difficult to receive systematic and professional risk assessment.
On the other hand, the difficulty of early detection of ovarian cancer does not mean that early screening should be given up. Experts suggest that it is necessary to carry out standardized cancer screening every year.
At the same time, women should pay attention to their own symptoms. If abdominal pain, abdominal distension, irregular vaginal bleeding, etc. occur, you should go to the hospital as soon as possible.
“By the time symptoms show up, it may be too late,” said Diane Miller, chief of the Gynecologic Oncology Unit at the University of British Columbia in Canada. “I used to have the idea that many ovarian cancers are preventable. Whether the fallopian tubes are cut during hysterectomy, uterine fibroids or tubal ligation for contraception.”
source:
1. Until There’s a Cure, Prevent Ovarian Cancer. OCRA
2. To Prevent Cancer, More Women Should Consider Removing Fallopian Tubes, Experts Say. The New York Times
3. Breast cancer screening guidelines for Chinese women (2022 edition). Chinese Research Hospital. 2022,09(2):6-13. DOI:10.19450/j.cnki.jcrh.2022.02.003
4. Screening for ovarian cancer is ruled out after trial found it did not reduce deaths. BMJ. 2021; 373. doi: https://doi.org/10.1136/bmj.n1223
5. Clinical comparative analysis of ovarian cancer risk in patients undergoing hysterectomy, bilateral salpingectomy and unilateral salpingectomy. PLA Journal of Preventive Medicine. Issue 2, 2019
6. Outcome and Management of Serous Tubal Intraepithelial Carcinoma Following Opportunistic Salpingectomy: Systematic Review and Meta-Analysis. Journal of Obstetrics and Gynaecology Canada. doi.org/10.1016/j.jogc.2022.08.018
7. Opportunistic salpingectomy at cesarean delivery in Japan: A questionnaire for registered physicians of the MFICU Liaison Council. Hypertension Research in Pregnancy. doi.org/10.14390/jsshp.HRP2021-007
8. Impact of the coverage of risk-reducing salpingo-oophorectomy by the national insurance system for women with BRCA pathogenic variants in Japan. Sci Rep. 13,1018(2023). https://doi.org/10.1038/s41598-023 -28304-w
9. Chinese expert consensus on prophylactic salpingectomy (2021 edition). Chinese Journal of Practical Gynecology and Obstetrics. August 2021, Volume 37, Issue 8
10. Outcomes From Opportunistic Salpingectomy for Ovarian Cancer Prevention. JAMA Netw Open. 2022;5(2):e2147343. doi:10.1001/jamanetworkopen.2021.47343
11. Risk-Reducing Salpingectomy: Let Us Be Opportunistic. Cancer. 2017 May 15;123(10):1714–1720. doi:10.1002/cncr.30528
Why are more and more women choosing to have their healthy fallopian tubes removed?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.