Intestinal flora may affect COVID-19 pneumonia and immune response
- Why Lecanemab’s Adoption Faces an Uphill Battle in US?
- Yogurt and High LDL Cholesterol: Can You Still Enjoy It?
- WHO Releases Global Influenza Vaccine Market Study in 2024
- HIV Infections Linked to Unlicensed Spa’s Vampire Facial Treatments
- A Single US$2.15-Million Injection to Block 90% of Cancer Cell Formation
- WIV: Prevention of New Disease X and Investigation of the Origin of COVID-19
Intestinal flora may affect COVID-19 pneumonia and immune response
Intestinal flora may affect COVID-19 pneumonia and immune response. GUT: The composition of the intestinal flora may affect the severity of COVID-19 and the immune response.
The intestine is the largest immune organ of the human body. Its resident microbiota can regulate the immune response of the host. There are about 10 trillion bacteria in the human intestine, which affect the body weight, digestion ability, resistance to infection and autoimmune diseases. The risk of illness, and even control the body’s response to cancer treatment drugs
The intestine is the largest immune organ of the human body. Its resident microbiota can regulate the immune response of the host. There are about 10 trillion bacteria in the human intestine, which affect the body weight, digestion ability, resistance to infection and autoimmune diseases. It can even control the body’s response to cancer treatment drugs.

On January 11, 2021, researchers from the Chinese University of Hong Kong published a research paper titled: Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19 in the top medical journal Gut.
The study shows that the type and number of bacteria in the intestine may affect the severity of COVID-19 and the degree of response of the immune system to infection, and the imbalance of microbiome composition may also be related to persistent inflammatory symptoms.
Between February and May 2020, researchers obtained blood and blood from 100 hospital inpatients confirmed to be infected with the COVID-19 virus in the laboratory and 78 uninfected patients who participated in microbiological studies before the pandemic. Stool samples and medical records.
The severity of patients is divided into 4 types. If there is no X-ray evidence of pneumonia, the severity is classified as mild; if pneumonia is found with fever and respiratory symptoms, it is moderate; if the patient finds it is difficult to breathe normally, it is severe; if the patient requires mechanical ventilation or requires Organ failure in intensive care is severe.
In order to describe the characteristics of the gut microbiota, 41 COVID-19 patients provided multiple stool samples during their hospitalization, of which 27 patients provided a series of stool samples within 30 days after the SARS-CoV-2 virus was cleared.
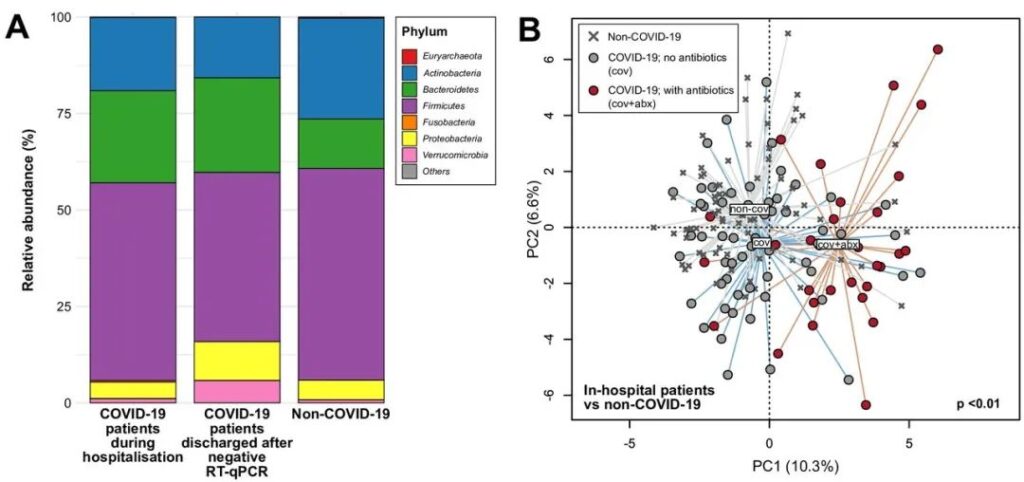
The analysis of all 274 stool samples showed that there are significant differences in the composition of the gut microbiome between patients with and without COVID-19, regardless of whether they have received drug treatment including antibiotics.
Compared with people without infection, patients with new coronavirus pneumonia have higher numbers of active rumen cocci and Bacteroides dosei. Moreover, they can affect the immune system response of much fewer types, such as Bifidobacterium adolescentis, Clostridium prasmodium and Eubacterium rectum.
Differences in composition of intestinal flora between COVID-19 and non-COVID-19 subjects
Taking into account the use of antibiotics and the age of the patient, lower numbers of Clostridium prasectii and Bifidobacterium are particularly related to the severity of the infection. In samples taken up to 30 days after the infected patient cleared the virus from the body, the number of these bacteria is still very small.
The new coronavirus infection prompts the immune system to produce inflammatory cytokines. In some cases, this response may be excessive, leading to extensive tissue damage, septic shock, and multiple organ failure.
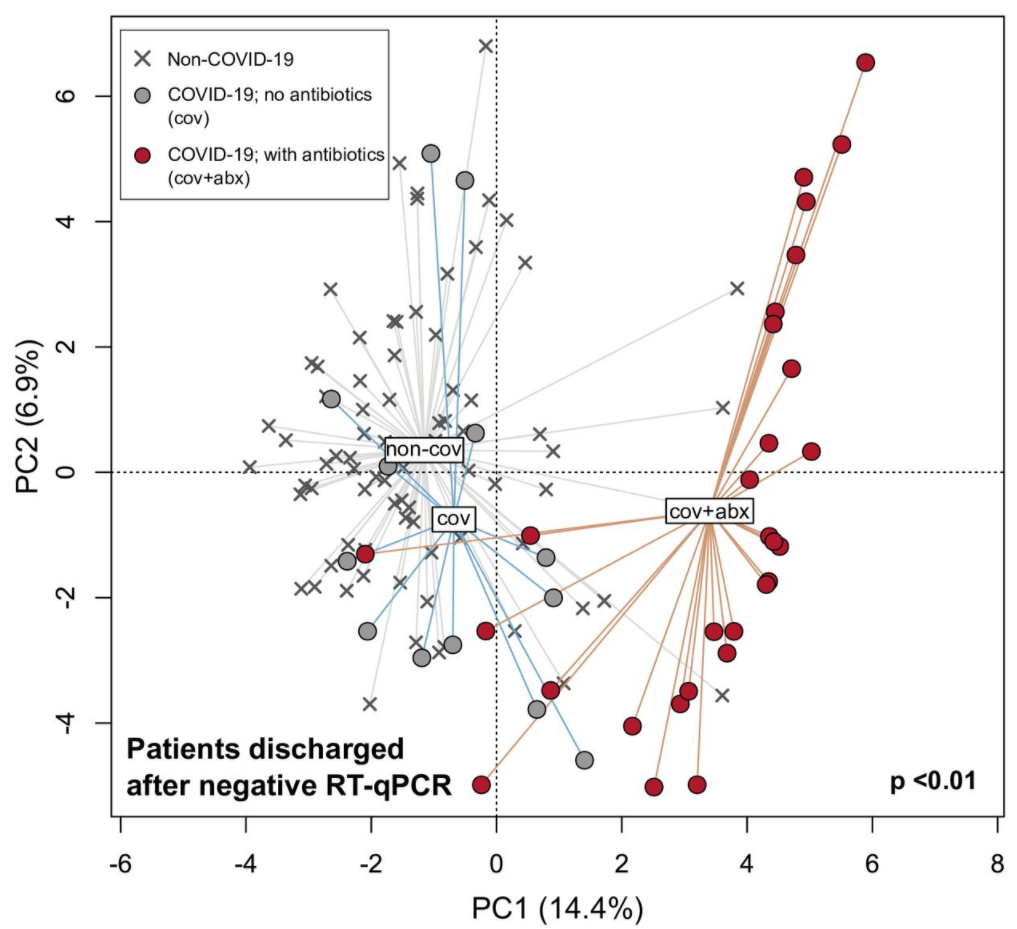
Principal component analysis of intestinal flora in patients with COVID-19 who have recovered or who have not received antibiotics compared with those who have not received COVID-19
Analysis of blood samples showed that the microbial imbalances found in patients with COVID-19 are also related to increased levels of inflammatory cytokines and blood markers of tissue damage (such as C-reactive protein and certain enzymes).
The researchers said that this suggests that the intestinal flora may affect the immune system’s response to the new coronavirus infection, and may affect the severity and outcome of the disease.
A recent study in The Lancet stated that 76% of patients with COVID-19 still had persistent symptoms 6 months after they were discharged from the hospital. The study evaluated the health status of patients with COVID-19 in Wuhan Jinyintan Hospital 6 months after discharge. , Found that 76% of patients still have at least one persistent symptom.

This study believes that poor intestinal flora may lead to immune-related health problems after infection with the new coronavirus.
The research team also said that this is an observational study, so the cause cannot be determined. The intestinal flora of different populations varies greatly. Therefore, the changes observed in the study may not be applicable to other COVID-19 patients elsewhere. .
In short, strengthening the beneficial intestinal bacteria consumed in the new coronavirus infection can be a new way to reduce severe symptoms. This study emphasizes the importance of managing the patient’s intestinal flora during and after treatment for the new coronavirus infection.
(sourceinternet, reference only)
Disclaimer of medicaltrend.org