Can people who have been infected with the flu virus resist COVID-19?
- Normal Liver Cells Found to Promote Cancer Metastasis to the Liver
- Nearly 80% Complete Remission: Breakthrough in ADC Anti-Tumor Treatment
- Vaccination Against Common Diseases May Prevent Dementia!
- New Alzheimer’s Disease (AD) Diagnosis and Staging Criteria
- Breakthrough in Alzheimer’s Disease: New Nasal Spray Halts Cognitive Decline by Targeting Toxic Protein
- Can the Tap Water at the Paris Olympics be Drunk Directly?
Can people who have been infected with the flu virus resist COVID-19?
- Should China be held legally responsible for the US’s $18 trillion COVID losses?
- CT Radiation Exposure Linked to Blood Cancer in Children and Adolescents
- FDA has mandated a top-level black box warning for all marketed CAR-T therapies
- Can people with high blood pressure eat peanuts?
- What is the difference between dopamine and dobutamine?
- How long can the patient live after heart stent surgery?
Can people who have been infected with the flu virus resist COVID-19? Scientists tell you another secret of COVID-19!
Introduction: Can people who have been infected with the flu virus resist COVID-19?
As the COVID-19 virus is raging around the world, all walks of life have taken positive actions. It is not only the government, medical staff, but also the scientific community that have made tremendous efforts. These scientists are actively conducting experiments to study the characteristics of the new coronavirus, so as to develop more effective ways to resist and treat habits. In the course of these studies, scientists have continued to make surprising discoveries.
Recently, scientists from Berlin made another horrifying discovery: People who have been infected with other coronaviruses before and have suffered from the common cold will have a certain degree of resistance to the new coronavirus. what the hell is it?
In medicine, the reaction of antibodies or sensitized lymphocytes with different antigens with the same or similar epitopes is called cross-reaction.
Because of the existence of the common antigen, the antibodies produced by the two kinds of cells stimulated by the body can not only bind to the corresponding epitopes on their own surface respectively, but the antibodies produced by the stimulated body by the A bacteria can also bind to the same epitopes on the surface of the B bacteria; Similarly, the antibodies produced by Bacteria stimulating the body can also bind to the same epitopes on the surface of A bacteria, but the degree of reaction is relatively weak. This kind of antigen and antibody reaction is called cross-reaction. The formation of cross-reaction phenomenon may be related to the following factors:
- Common antigen, some biological macromolecules of different organisms have the same antigen structure;
- Common epitope, some fragments (peptides) of different biological macromolecules have the same epitope;
- Similar epitopes, different biological macromolecules, part of the spatial conformation of the epitopes is very similar, which can fit the complementarity determining region of the same antibody.
The new discoveries of Berlin scientists to be described in this article are inseparable from the principle of cross-reaction.
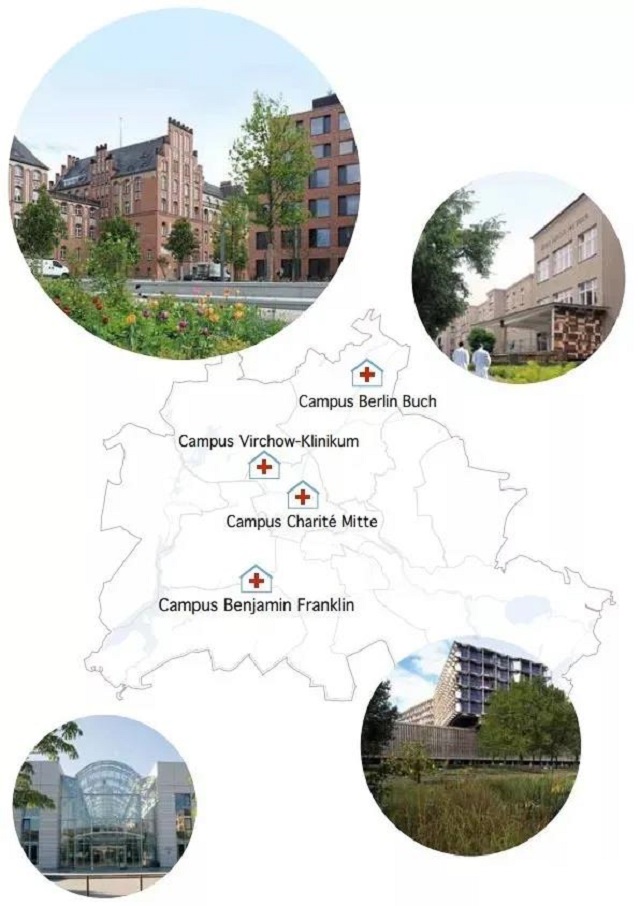
The picture shows Charretti Berlin Medical University
Researchers from Charretti Berlin Medical University (Charité – Universitätsmedizin Berlin) [1], the Berlin Institute of Health, and the Max Planck Institute for Molecular Genetics have found through their latest study: For those who have been infected by a certain type of coronavirus before People with the common cold have certain immune cells in their bodies that can help them enhance their immune response to the new coronavirus. This immune function can compare to them whether during natural infection or after vaccination. Others have better defenses against the new coronavirus. They published the results of this research in an article titled “Cross-reactive CD4+ T cells enhance SARS-CoV-2 immune responses upon infection and vaccination” in “Science” magazine:

In research and experiments, they also found that: this “immune cross-reaction ability” will slowly decline with age. This feature helps researchers explain why the elderly are more susceptible to serious diseases and why they are often weaker in immunity after being vaccinated than young people.
Last year, researchers at Charretti Berlin Medical University and the Max Planck Institute for Molecular Genetics were shocked to discover that some people who have not been infected with the new coronavirus actually have immune memory cells that can help them recognize the new coronavirus, and These scientists reported this discovery for the first time.
They then came to this conclusion:
The reason why these T helper cells can be generated in these people who have not been infected with COVID-19 is because these people must have been infected with other coronaviruses before; however, those who have previously infected them.
Most of the viruses are harmless, which means that they will not cause a big impact on life; because the structure of those coronaviruses is similar to the current new coronaviruses, (especially the characteristics of the spike protein located on the outer surface of the coronaviruses and the new coronaviruses The spike protein properties of T-helper cells are very similar), these T helper cells will also attack the new coronavirus like other coronaviruses.
This “cross-reaction” hypothesis has been fully confirmed through a variety of experiments by scientists.
However, whether these immune cells will affect the follow-up process of the new coronavirus infection is still unclear, and it is also one of the subjects of intense debate in the scientific community. Dr. Lucie Loyal is the first author of this paper and a researcher at Charretti Berlin Medical University and the Berlin Health Institute Regenerative Therapy Center. She explained: “Our assumption at the time was that people involved in this cross-reaction T helper cells have a certain protective effect on the human body and can play a role in resisting viral infections.
Therefore, those who have previously been infected with the epidemic coronavirus (ie: the long-existing and widely spreading coronavirus) will have symptoms when they are infected with the new coronavirus. It will be weakened. However, in some cases, the facts may be just the opposite. If people are infected with certain viruses (involving similar strains) a second time, it will easily lead to a false immune response and negatively affect the clinical medical process. Influence and bring about negative effects.”
In the current study, the Berlin research team provided evidence to support their previous assumptions about the existence of protection. According to their data, immune cross-reaction may not only be one of several potential reasons for changes in the severity of the COVID-19 disease, but also help explain why the efficacy of the vaccine varies among different age groups.
The quality of the immune response to the new coronavirus, that is, the strength of the immune response, is related to the number of cross-reactive cells that existed in the body before the new coronavirus was infected. These T helper cells are particularly effective in recognizing specific regions of the spike protein. Because the genetic sequences of the epidemic coronavirus and the new coronavirus are very similar and have been well preserved, the specific region of this spike protein can be easily identified.
In the current study, the researchers recruited some people who had not been infected with COVID-19 virus before, and regularly performed nucleic acid tests on them to check whether they were infected with COVID-19. Starting in mid-2020, 17 of the nearly 800 participants they recruited have tested positive. Researchers immediately conducted detailed observations and analyses of the immune systems of these COVID-19 patients.
Through analysis, they found that one of the factors that determine whether an individual has a certain immune response to the new coronavirus is: the role of T helper cells-if the new coronavirus patient has been infected by other common cold viruses before, then T Helper cells have already been generated, and these cells can now play a major immune role in fighting the new coronavirus.
The quality of the immune response to the new coronavirus, that is, the strength of the immune response, is related to the number of cross-reactive cells that existed in the body before the new coronavirus was infected. These T helper cells are particularly effective in recognizing specific regions of the spike protein. Because the genetic sequences of the epidemic coronavirus and the new coronavirus are very similar and have been well preserved, the specific region of this spike protein can be easily identified.
Dr. Claudia Giesecke-Thiel, the corresponding author of this paper and the head of the flow cytometry service team of the Max Planck Institute of Molecular Genetics, explained: “During infection with other harmless coronaviruses, the immune system will establish a A protective universal memory of the’coronavirus’.
Once infected with the new coronavirus, these memory cells will be reactivated and initiate a response to newly invading pathogens. This will help to accelerate the initial immune response to the new coronavirus, and In the early stages of infection, the spread of the virus can be suppressed, thus playing an important and positive role in the treatment process of the disease.
This does not mean that people who have been infected with the common cold virus must be protected from the new coronavirus infection, but also It will not change the current status of the new coronavirus pandemic. There is no doubt that there are not a few people who have been infected with other coronaviruses before, but they are also infected with the new coronavirus. From this point of view, this does not reduce the importance of vaccination.
Our research The results provide an explanation for our observations of patients since the outbreak, and explain to a certain extent why patients with COVID-19 are also patients with COVID-19, but the symptoms of infection are very different between individuals.
This further confirms that the resistance and immunity of T cells generated by the cross-reaction to the virus will also be enhanced after vaccination with the COVID-19 vaccine. Just like a natural infection, the vaccine promotes the production of the spike protein of the new coronavirus in the body (including its well-preserved parts) and provides these spike proteins for the immune system.
We analyzed the immune response of the 31 healthy people. After vaccinating them, their immune system reacted differently from before the vaccination. The difference between before and after shows that normal T helper cells need to be vaccinated after vaccination.
It is gradually activated within two weeks; however, the activation of cross-reactive T helper cells is very rapid and can be activated within a week. Of course, this also has a particularly positive effect on the production of antibodies. This speeds up the production of antibodies, so that after the first dose of vaccine, people can produce antibodies against the remaining part of the spike. This antibody is usually produced after vaccination booster shots. “
Even after vaccination, if the person has been infected with other influenza coronaviruses before, at least part of the immune memory can be used. This explains well why after people were vaccinated with the COVID-19 vaccine for the first time, among young people, the immunity and protection brought by the vaccine were produced so quickly.
Not only that, but the protection is also very strong. . In the second part of the scientist’s study, the researchers analyzed the T helper cells of about 570 healthy individuals, and they observed that the immune cross-reactivity of the elderly is gradually decreasing.
In fact, in these elderly people, the number of cross-reactive T cells and their ability to bind pathogens are much weaker than those in young people. This decline in immune cross-reactivity is normal, which is caused by age-related changes.
Professor Thiel said: “Infection with influenza coronavirus is good for young people because it will help them weaken the damage caused by the new coronavirus. Unfortunately, this benefit does not play a big role in the elderly. The third dose (booster) will be able to compensate for this weak immune response and ensure that this high-risk group has sufficient immunity to the new coronavirus.”
[1] The Charretti Medical University of Berlin has a strong tradition and is also the largest university-affiliated teaching hospital in Europe. It was established as a quarantine hospital outside Berlin in 1710. After a century, the clinic was completely rebuilt and became the medical department of the newly established University of Berlin.
It has four campuses. Adhering to the motto of “research, teaching, treatment, and help”, academic teaching, research and patient care have become an inseparable whole. In Germany, it is a medical school with the same reputation as Heidelberg University.
Can people who have been infected with the flu virus resist COVID-19?
(source:internet, reference only)
Disclaimer of medicaltrend.org
Important Note: The information provided is for informational purposes only and should not be considered as medical advice.



